Authored By:
Jamie Furstein, PhD, DNAP, CRNA
Associate Professor University of Cincinnati School of Nurse Anesthesia

Overview
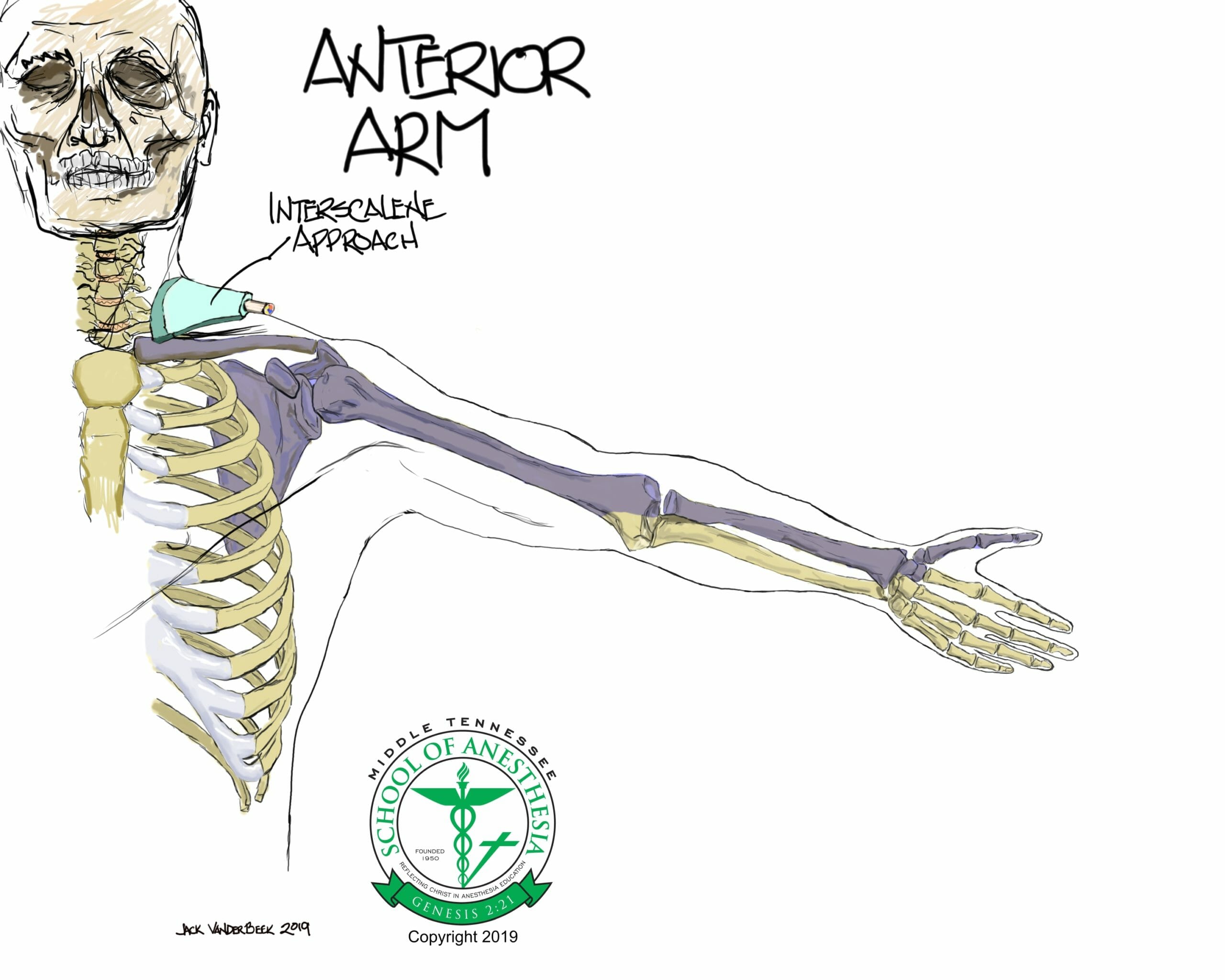
The brachial plexus supplies all the motor and most of the sensory functions of the shoulder, with the exception of the cephalad cutaneous areas of the shoulder.
-
- The cephalad cutaneous areas of the shoulder are innervated by the supraclavicular nerves which originate from the superficial cervical plexus (C3-C4).
The terminal branches of the brachial plexus that supply the majority of the shoulder innervation are the axillary and suprascapular nerves.
-
- The axillary nerve originates from C5-C6 nerve roots, with occasional contribution from C4. It is derived from the posterior cord of the brachial plexus.
- The suprascapular nerve supplies sensory innervation to the subacromial bursa, acromioclavicular joint, coracoclavicular ligament, and 70% of the shoulder joint capsule. This nerve arises from the superior trunk of the brachial plexus, C5-C6 and possibly C4.
Indications
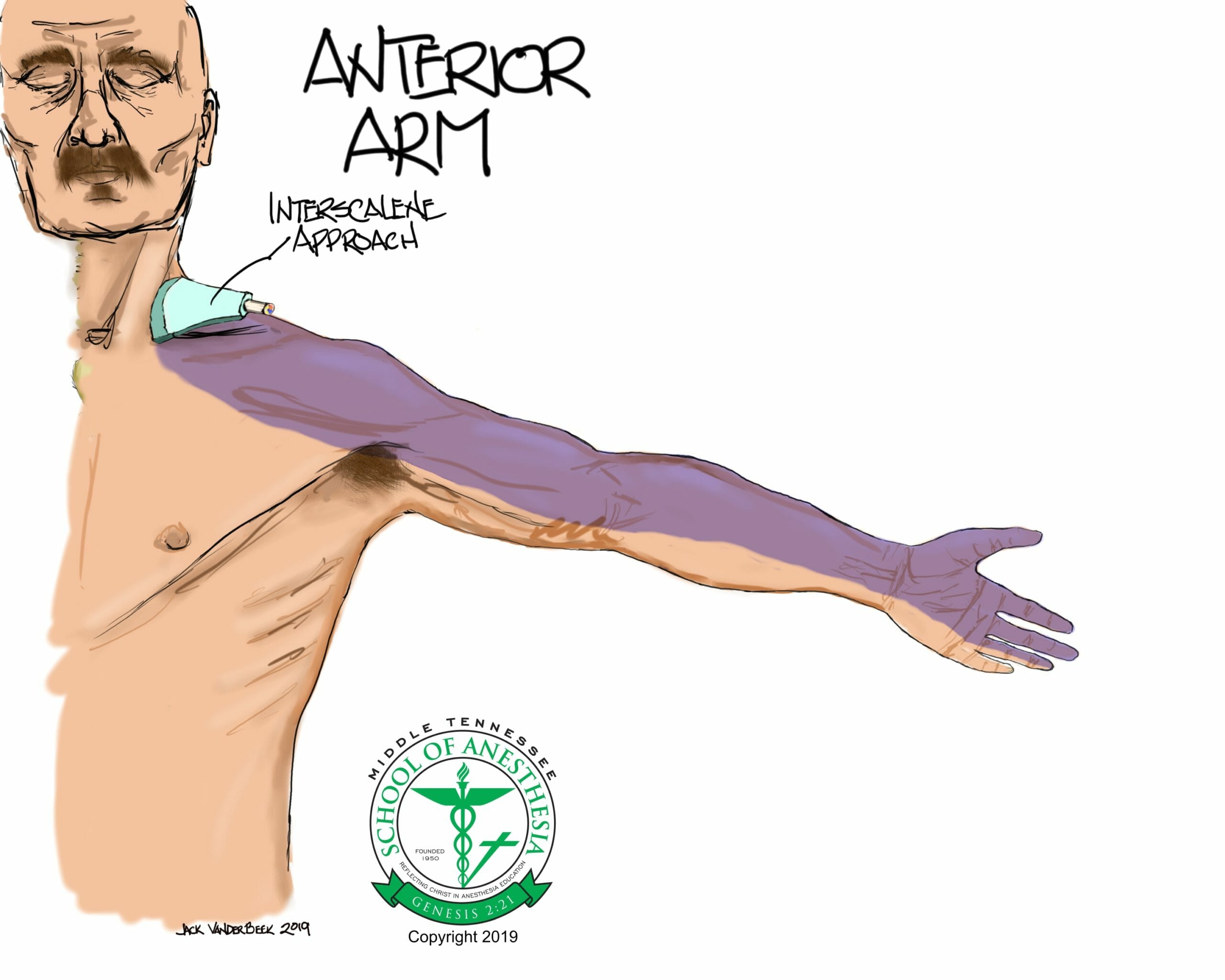
- The interscalene approach to the brachial plexus is particular well suited for operations on the shoulder, the clavicle, or the upper arm.
- The interscalene approach to the brachial plexus primarily anesthetizes the C5-C7 nerve roots, with variable proximal spread to the cervical plexus (C3-C4).
- Because the ulnar nerve is derived from the C8-T1 nerve roots and is frequently “spared” with an interscalene block, this technique is ineffective for surgeries involving the hand.
Positioning
- Supine, high or low Fowler’s position with the patient’s head turned slightly to contralateral side.
- If performing interscalene brachial plexus blockade with the patient on a stretcher, consider placing a bolster behind the patient’s back to allow more room for advancing the needle from a posterolateral direction.
Anatomy
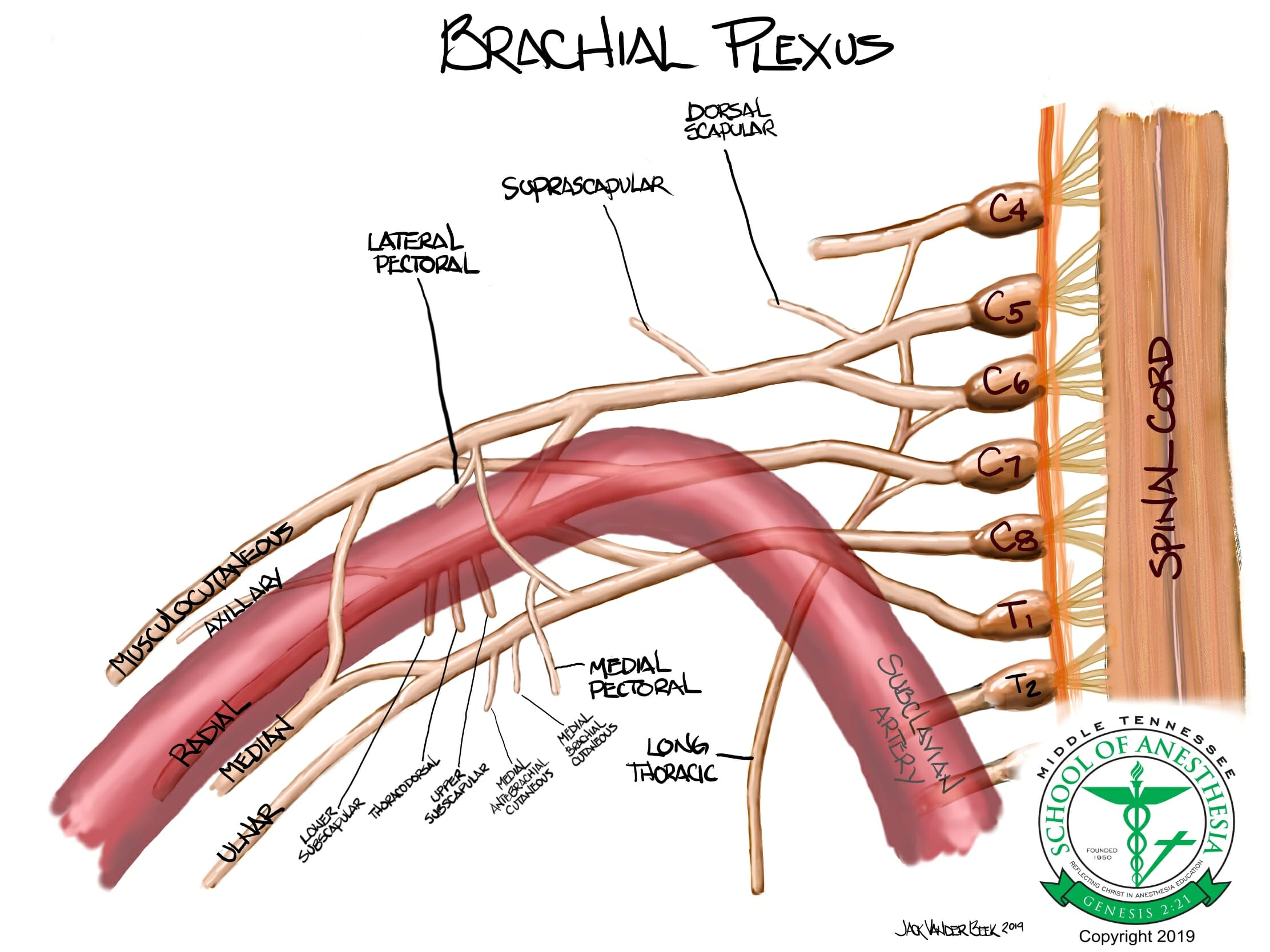
The brachial plexus can be divided into FIVE distinct sections based on anatomic structure and location.
These sections are the:
-
-
- Roots
- Formed at each vertebral level by paired spinal nerves C5, C6, C7, C8, and T1 (sometimes there are contributions from C4 and T2). They leave the spinal cord via the intervertebral foramina of the vertebral column and divide into anterior and posterior nerve fibers. The roots of the brachial plexus are formed by the anterior divisions of spinal nerves C5-T1 (the posterior divisions go on to innervate the skin and musculature of the trunk).
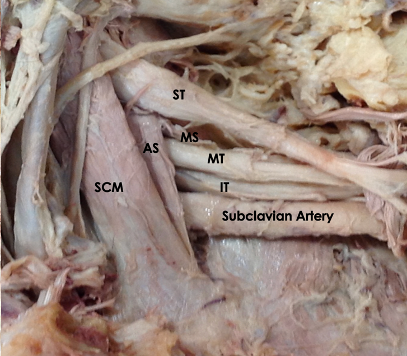
- Trunks
- These roots merge to form three trunks: “superior” or “upper” trunk (C5-C6), “middle” trunk (C7), and “inferior” or “lower” trunk (C8, T1).
- Divisions
- Each trunk then splits in to form six divisions: the anterior divisions of the upper, middle, and lower trunks and the posterior divisions of the upper, middle, and lower trunks.
- Cords
- The cords are named by their position with respect to the axillary artery. The posterior cord is formed from the three posterior divisions of the trunks (C5-C8,T1). The lateral cord is the anterior divisions from the upper and middle trunks (C5-C7). The medial cord is simply a continuation of the anterior division of the lower trunk (C8,T1).
- Terminal branches
- Musculocutaneous nerve
- Axillary nerve
- Median nerve
- Radial nerve
- Ulnar nerve
- Roots
-
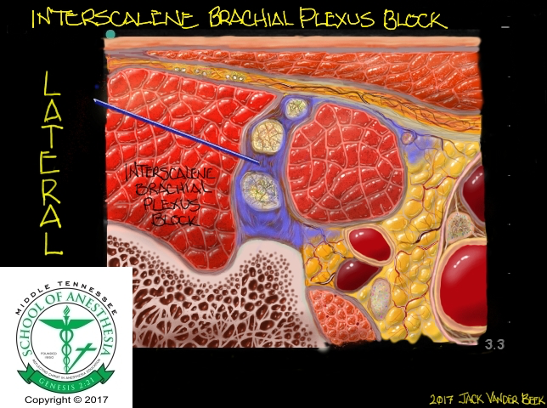
As the brachial plexus travels out from the cervical spine it is enveloped in a neurovascular sheath that is an extension of the prevertebral and scalene fascia. The prevertebral layer of cervical fascia splits to invest the anterior and middle scalene muscles and then fuses at the lateral edges, effectively creating a tubular sheath through which the entire brachial plexus travels. This sheath is the anatomical basis for brachial plexus peripheral nerve blocks as covers the brachial plexus from the intervertebral foramina all the way through the terminal branches.
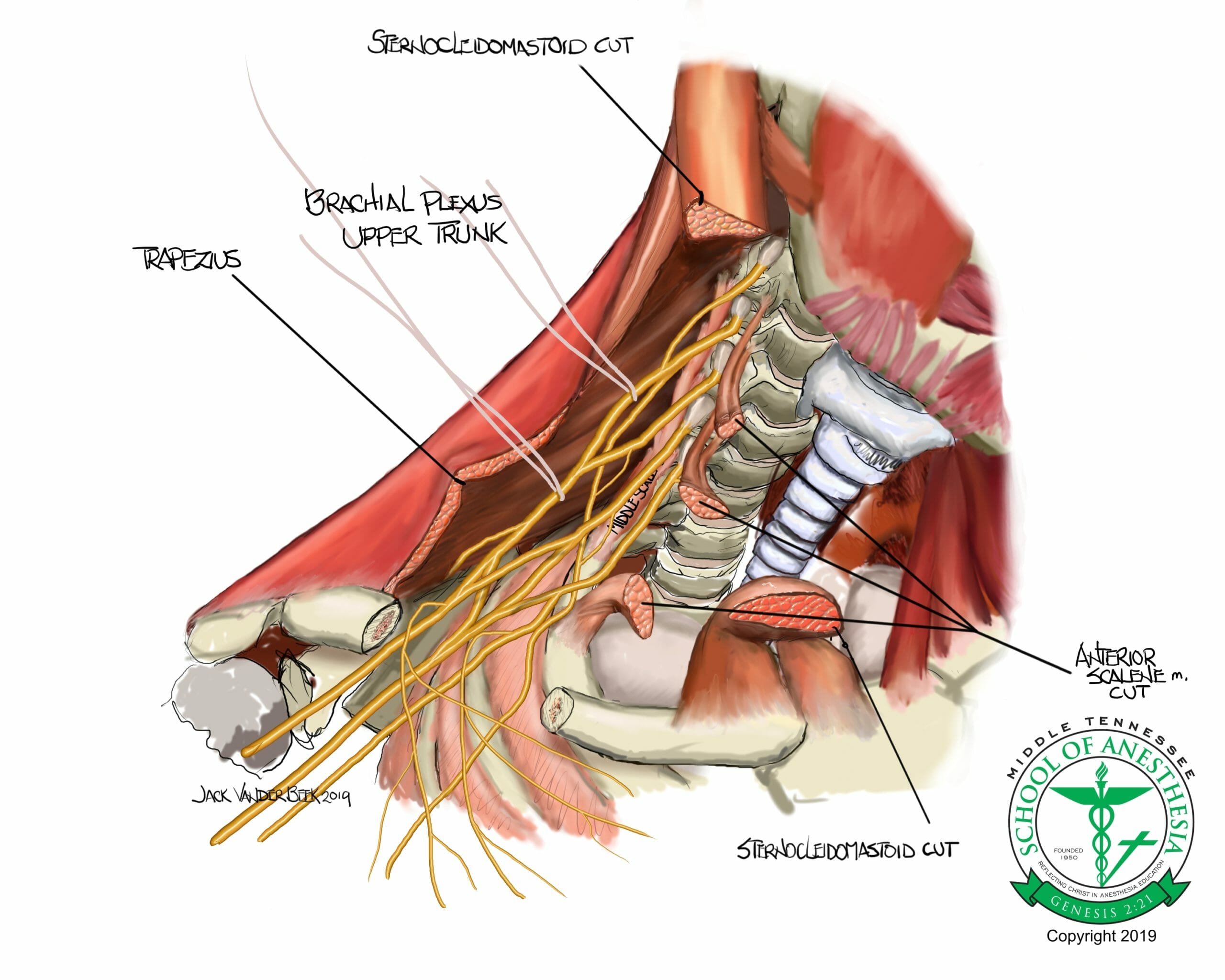
From an anatomical standpoint, the nerves of the brachial plexus emerge from their respective intervertebral foramina and course posterior towards the vertebral artery, ultimately passing between the anterior and middle scalene muscles as the trunks of the brachial plexus.
The interscalene block is performed at the level of the cricoid cartilage, which equates to C6, where the nerve roots emerge from between the anterior and middle scalene muscles.
The lateral border of the clavicular head of the sternocleidomastoid is the ideal location for interscalene brachial plexus blockade as the brachial plexus is superficial and easily identified in this location.
Dermatome Coverage
Scanning Technique
- A high-frequency (>12 MHZ) linear array should be used when performing interscalene brachial plexus blockade.
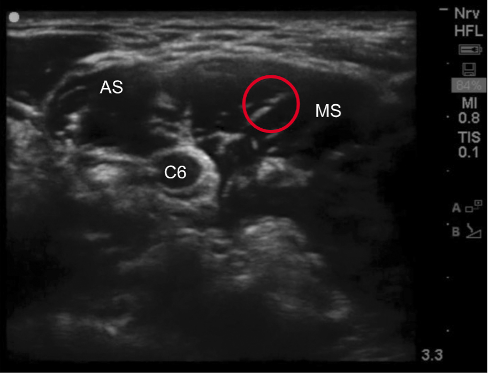
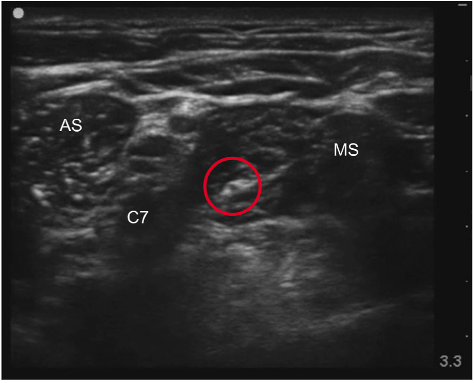
- Placing the probe in an oblique plane may offer the best transverse view of the brachial plexus. In this position, the nerves of the brachial plexus will be displayed as hypoechoic structures with hyperechoic rings.
- Position the probe on the lateral aspect of the neck at the level of the cricoid cartilage (C6), perpendicular to the brachial plexus and centered over the interscalene groove.
- It may be helpful to first locate the brachial plexus in the supraclavicular fossa, where the plexus can be found lateral to the subclavian artery. Trace the brachial plexus cephalad until the anterior and middle scalene muscles are seen surrounding the brachial plexus.
- An alternate approach to identifying the brachial plexus in the interscalene groove is to start by placing the probe near the cricoid cartilage. Starting in this position, move the probe laterally to visualize the carotid artery, internal jugular vein, and sternocleidomastoid muscles. Ultimately, the anterior and middle scalene muscles will be visualized surrounding the brachial plexus in the interscalene groove.
Sonoanatomy
Needle Approach
- While both in-plane and out-of-plane approaches can be used for interscalene brachial plexus blockade, an in-plane approach is most advisable.
- If using an in-plane approach, the needle should be inserted in a lateral-to-medial fashion to avoid puncturing the carotid artery and/or jugular veins.
- the medial-to-lateral in-plane approach increases the potential of injury to the phrenic nerve as it may lie in the path of the needle trajectory.
- Although an out-of-plane approach provides a shorter, more direct path to neural targets, this approach does not allow continuous imaging of the entire needle shaft and tip during needle advancement.
- In the interscalene groove, the brachial plexus will appear like a “stoplight”, with the nerve roots of C5, C6, and C7 stacked on top of each other between the anterior and middle scalene muscles.

Injection Technique
- The target for local anesthetic deposition is between C5 and C6. Attempts should not be made to inject local anesthetic between what is perceived to be C6 and C7.
-
- Cadaver studies have reported that the “stoplight” sign is made up of the root of C5, the upper fascicle(s) of C6, and the lower fascicle(s) of C6 without contribution from C7. Therefore, attempted injection of local anesthetic between what is commonly perceived as the space between C6 and C7 would be an intraneural injection at C6, which could potentially spread toward the neuraxial space.
- Following injection, local anesthetic will be visualized surrounding the brachial plexus, separating the plexus from the scalene
- Do not attempt to advance the needle beyond the brachial plexus in an attempt to place local between the anterior scalene muscle and brachial plexus as neural injury is likely to occur. Demanding an aggressive circumferential spread of local anesthetic not only increases the likelihood of needle-to-nerve trauma, but often requires more repositioning of the needle and the incidence of unnecessary
Nerve Stimulator Guidance
Flexion or extension of the wrist, external or internal rotation of the wrist, movement of fingers, flexion of the elbow are all twitch responses of terminal nerves of the brachial plexus. The elicitation of these twitches at 0.3-0.5 mA range and loss of these twitch responses at 0.2 mA indicate a proper location of the needle tip within the brachial plexus neural sheath and not in an intraneural location.
Direct stimulation of the phrenic nerve can cause diaphragm elevation and requires redirection of the needle tip to a more lateral and deeper location. Stimulation of the dorsal scapular (scapular elevation) and accessory (trapezius- movement of the neck) nerves also require redirection of the needle until a terminal, brachial plexus motor response is elicited.
Local Anesthetic Volume
Interscalene Block: 15-20 ml
- Decreasing the volume injected from ~30 mLs to ~15 mLs decreases the incidence of a paralyzed hemidiaphragm from ~90% to ~22%, however, no single intervention to date has proven to reliably decrease its incidence below 20%.
- Commonly used local anesthetics include bupivacaine and ropivacaine, with concentrations varying between 0.2-0.5%.
- Commonly used local anesthetics include bupivacaine and ropivacaine, with concentrations varying between 0.2-0.5%.
- A number of additives such as clonidine, dexmedetomidine, and dexamethasone have been reported to prolong the duration of analgesia.
- Perineural dexmedetomidine has been reported to improve the onset, quality, and duration of analgesia. These benefits, however, should be weighed against the increased risks of motor blockade prolongation and transient bradycardia and hypotension.
- Perineural dexamethasone in combination with local anesthetic has been reported to prolong analgesia more effectively than the combination of intravenous dexamethasone and interscalene blockade.
- Combining clonidine and dexamethasone with local anesthetic has the potential to significantly increase the duration of action when compared to local anesthetic alone.
- The evidence supporting the use of liposomal bupivacaine in interscalene brachial plexus blockade is promising, but its superiority is yet to be determined when compared to single-injection or continuous perineural infusions using unencapsulated (standard) long-acting local anesthetics.
Block Complications
- Contraindications include those patients who cannot tolerate 25% decrease in pulmonary function due to possible anesthetic blockade of the phrenic nerve or have a contralateral hemidiaphragmatic paresis that could result in complete respiratory failure.
- Peripheral nerve damage
- Hematoma
- Hemidiaphragmatic paresis (phrenic nerve)
- Horner syndrome
- Horner syndrome results from blockade of the stellate ganglion block resulting in interruption of the sympathetic pathway.
- Symptoms include:
- Ptosis
- Miosis
- Anhidrosis
- Flushed cheek
- Nasal congestion
- Hoarse voice (recurrent laryngeal nerve)
- Phrenic nerve palsy:
- Ipsilateral paralysis of the diaphragm
- Shortness of breath
- Hiccups
- Clinical symptoms may persist for the duration of the block, though often subside within 2-4 hours. No intervention is required; however, patients should be reassured the symptoms are transient and self-limited.
- Local anesthetic toxicity (LAST)
- Epidural/spinal injection
- Pneumothorax
- Seizures: 1-2 ml injected into the arterial circulation above the clavicle can result in this complication.
- The vertebral artery enters the vertebral column at the level of C6, increasing the risk of intervascular injection. The vertebral artery, however, is not the sole branch of subclavian artery that is of concern as the thyrocervical trunk gives rise to the inferior thyroid, suprascapular, and transverse cervical arteries. The transverse cervical artery continues to divide into the superficial cervical and dorsal scapular arteries. While many resources note the presence of the vertebral artery relative to the brachial plexus, few images have been offered depicting the proximity of the superficial cervical artery. Once the transverse cervical artery bifurcates, the superficial cervical artery courses superficially and laterally across the anterior scalene muscle often crossing through or superficial to the trunks of the brachial plexus. Given the hypoechoic appearance of both vessels and the brachial plexus, the superficial cervical artery may be mistaken to be part of the brachial plexus by the novice clinician.
- A Doppler Color scan in the area of the needle path is warranted before placing an interscalene block in identifying any aberrant vessels present in the area.
PEARLS
- Extensive rotation to the contralateral side may distort images as muscle orientation will be altered.
- The external jugular vein is very superficial and easily compressed by the weight of the probe. Typically, it is located at the tip of the sternocleidomastoid and should be identified prior to needle insertion to avoid unintentional vascular puncture.
- Tilting the probe 10 20 degrees cephalad often improves image quality.
- Prior to injection, always assess the entire image for pulsating vessels with Doppler ultrasound.
- Aspirate frequently during injection and inject in small, 3-5 ml aliquots of volume.
- Stop injecting if the solution is not seen accumulating in the space around the nerve. Aspirate and adjust the ultrasound probe to make sure the injectate is within the area of survey.
- If there is excessive resistance to injection, either withdraw the needle slightly or advance if, depending on what is seen on the survey window and whether the patient complains of paresthesias.
- The space between the scalene muscle will only hold a given volume of solution. When the injected solution is seen passing over the superficial border of the anterior scalene muscle, the capacity of the interscalene space had been exceeded and injection should stop.
- Skin infiltration of the posterior arthroscopic port insertion site with local anesthetic is often necessary despite a successful interscalene block.
- The dorsascpaular nerve, which originates proximally from the C5 nerve root, and the suprascapular nerve (Superior truck) are not part of the brachial plexus and may require separate blockade if more distal approaches to the interscalene brachial plexus block are used.
- The dorsal scapular and long thoracic nerves will often traverse the middle scalene muscle and appear as hyperechoic structures on ultrasound. Before placing an interscalene block, an ultrasound scan should be done to evaluate the presence of these nerves in the middle scalene muscle, especially since they often lie in the direct needle path if an in-plane, lateral-to-medial needle approach is used by the regionalist. The use of a stimulator during the block performance could facilitate recognition and avoidance of these nerves in avoiding a mechanical nerve injury from needle contact.
References
- Chong, Matthew Alan, et al. “Perineural versus intravenous dexamethasone as an adjuvant for peripheral nerve blocks: a systematic review and meta-analysis.” Reg Anesth Pain Med 3 (2017): 319-326.
- Franco, Carlo D., and James M. Williams. “Ultrasound-guided interscalene block: reevaluation of the “stoplight” sign and clinical implications.” (2016): 452-459.
- Gabriel, Rodney A., and Brian M. Ilfeld. “An Updated Review on Liposome Bupivacaine.”Current Anesthesiology Reports(2019): 1-5.
- Hadzic, Admir.Hadzic’s textbook of regional anesthesia and acute pain management. McGraw Hill Professional, 2017.
- Hebl, James R., and Robert L. Lennon, eds.Mayo Clinic Atlas of Regional Anesthesia and Ultrasound-Guided Nerve Blockade. Oxford University Press, 2010.
- Ihnatsenka, Barys, and André P. Boezaart. “Applied sonoanatomy of the posterior triangle of the neck.” International journal of shoulder surgery3 (2010): 63.
- Kahn, Richard L., et al. “Perineural low-dose dexamethasone prolongs Interscalene block analgesia with bupivacaine compared with systemic dexamethasone: a randomized trial.” (2018): 572-579.
- Saied, Nahel N., et al. “Dexamethasone and clonidine, but not epinephrine, prolong duration of ropivacaine brachial plexus blocks, cross-sectional analysis in outpatient surgery setting.”Pain Medicine 10 (2016): 2013-2026.
- Sehmbi H, Shah UJ. In-plane interscalene block: A word of caution.J Anaesthesiol Clin Pharmacol. 2015;31(1):129–130. doi:10.4103/0970-9185.150574
- Spence, B. C., et al. “Ultrasound‐guided interscalene blocks: understanding where to inject the local anaesthetic.”Anaesthesia 6 (2011): 509-514.
- Tran, De QH, et al. “Diaphragm-sparing nerve blocks for shoulder surgery.”Regional Anesthesia & Pain Medicine 1 (2017): 32-38.
- Vandepitte, Catherine, et al. “Addition of liposome bupivacaine to bupivacaine HCl versus bupivacaine HCl alone for interscalene brachial plexus block in patients having major shoulder surgery.” (2017): 334-341.
- Vorobeichik, L., R. Brull, and F. W. Abdallah. “Evidence basis for using perineural dexmedetomidine to enhance the quality of brachial plexus nerve blocks: a systematic review and meta-analysis of randomized controlled trials.” BJA: British Journal of Anaesthesia2 (2017): 167-181.
- Kim YD, Yu JY, Heo HJ, Kim H. “Risk of encountering the dorsal scapular and long thoracic nerves during ultrasound-guided brachial plexus block with nerve stimulator.” Korean J of Pain. 2016;29(3):179-184.