Authored by:
Christian R. Falyar, DNAP, CRNA
Assistant Professor Duke University School of Nurse Anesthesia

Overview
- The TAP block is a fascial plane block in which local anesthetic is deposited in the fascial plane deep to the internal oblique (IOM) and superficial to the transversus abdominis (TAM) muscle providing somatic coverage of the abdominal wall and the parietal peritoneum.
- The TAP block does not provide visceral abdominal coverage.
Indications
A multimodal analgesic alternative for mid to low abdominal wall surgery when spinal or epidural anesthesia and/or intrathecal opioids are contraindicated or refused. Common procedures include cesarean section, laparoscopic abdominal procedures, open appendectomy, radical prostatectomy, gynecologic surgeries and hernia repair.
Positioning
Supine
Anatomy of the Abdominal Wall
The transversus abdominis plane (TAP) is the fascial plane between the IOM and TAM where the thoracolumbar nerves (T6-12) are located. The TAM is the innermost muscle of the anterior abdominal wall. It extends anteriorly from the aponeurosis of the of the linea alba to the aponeurosis of the thoracolumbar fascia posteriorly.
- Relevant Muscles of the Anterior Abdominal Wall
- The external oblique muscle (EOM) is the largest and most superficial muscle. It extends inferomedial from the lower eight ribs and attaches to the anterior iliac crest. Anteriorly, the aponeurosis of the EOM joins the aponeuroses of the other abdominal wall muscles to form the linea alba. Inferiorly, the aponeurosis of the EOM forms the inguinal ligament.
- The IOM originates from the iliac crest and thoracolumbar fascia and ascends superiorly in a perpendicular orientation to the EOM and attaches into the cartilages of the lower six ribs covering the anterolateral portion of the abdomen. Anteriorly, the aponeurosis joins with aponeuroses of the other abdominal wall muscles to form the linea alba.
- The TAM is the innermost of the three muscle layers. It arises from the cartilages of the lower five ribs, the iliac crest and thoracolumbar fascia. As its name implies, the TAM courses in a transverse direction; anteriorly, the aponeurosis is more lateral than the other muscles before becoming part of the linea alba and attaching to the pubic tubercle.
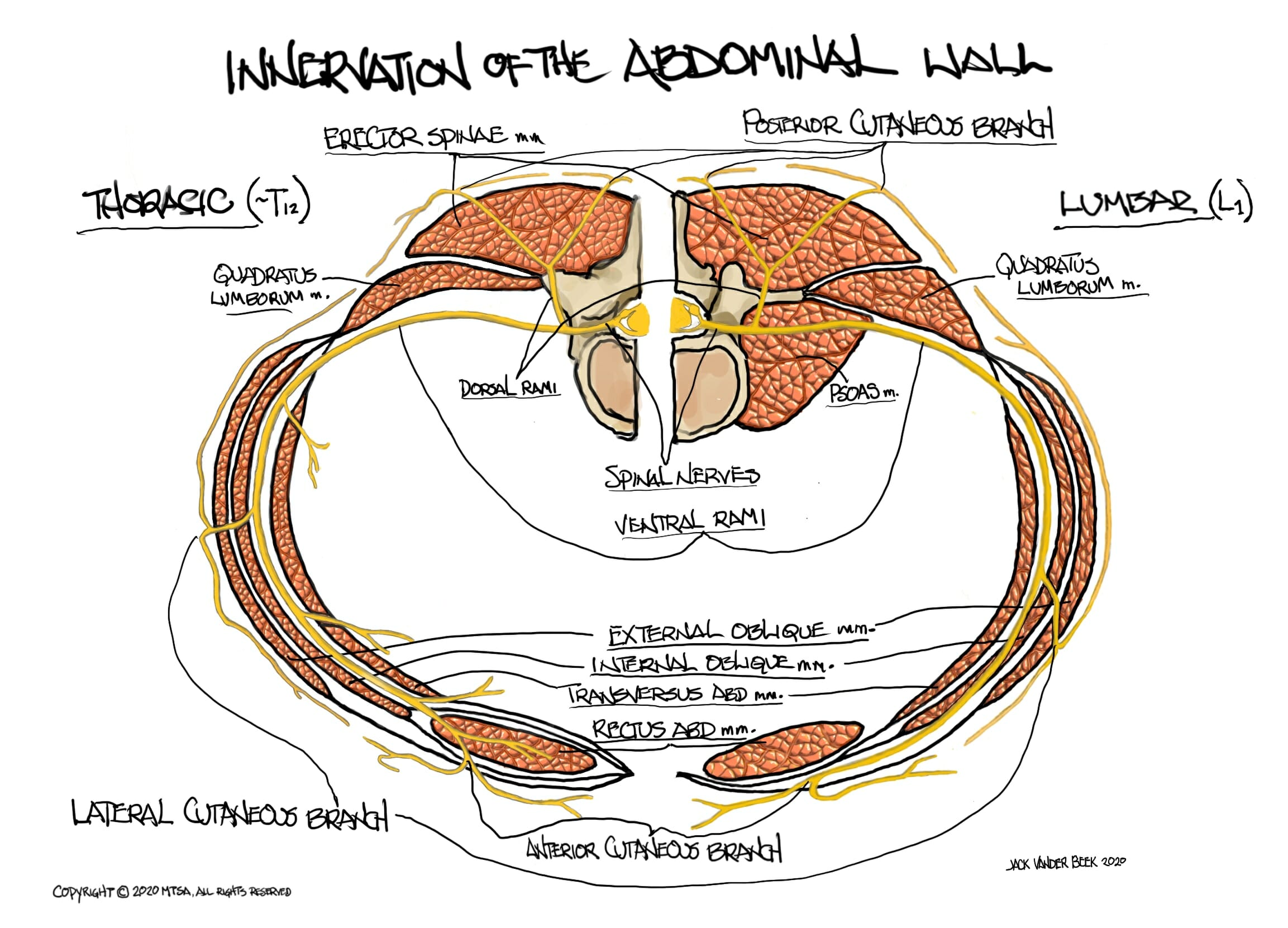
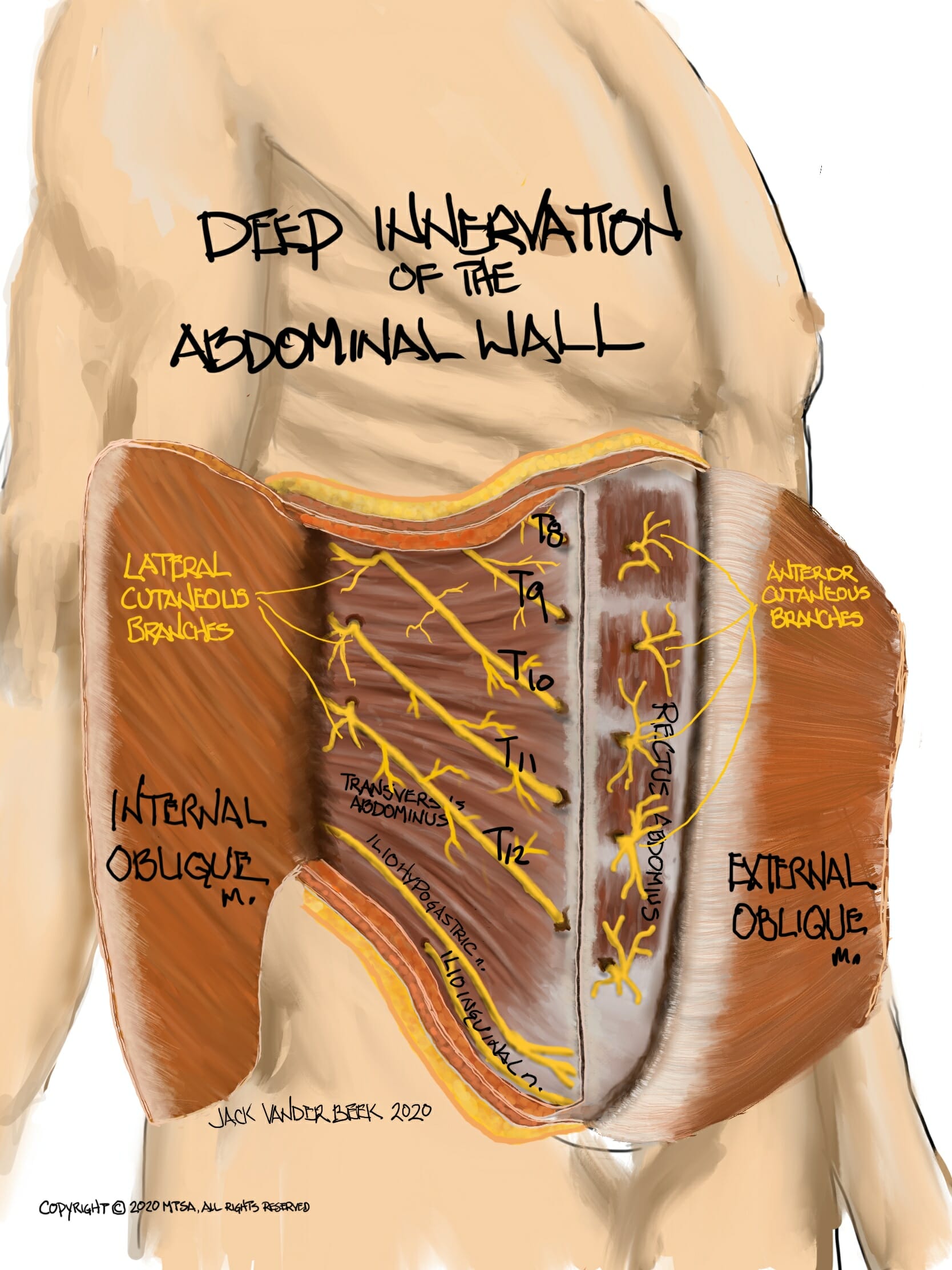
- Nerve Innervation of the Thoracoabdominal Wall
- The thoracoabdominal spinal nerves T6-T11 originate from the anterior rami of the spinal nerves and travel along their associated intercostal space, passing beneath the costal cartilage before entering the fascial plane between the TAM and IOM. They continue until they pierce the rectus abdominis muscle.
- A lateral cutaneous branch arises from the spinal nerves near the mid-axillary line and travel posteriorly, piercing the EOM to supply innervation to the skin of the lateral abdomen and back.
- The spinal nerves ultimately terminate in the rectus abdominis, where the become anterior cutaneous branches supplying sensation to the anterior abdomen.
- T12 is often referred to as the subcostal nerve. It is a large nerve that courses along the inferior border of T12 before passing under the lumbocostal arch.
- The iliohypogastric and ilioinguinal nerves (T12-L1) are classically described as the terminal branch of L1 with occasional innervation from T12. However, there is significant variability among individuals, with reports of L2-L3 innervation in up to 20% of individuals. Both nerves emerge from the psoas major and course inferolaterally along the ventral surface of the quadratus lumborum muscle (QLM) and TAM parallel and superior to the iliac crest.
- The iliohypogastric nerve enters earlier than the ilioingual nerve at the anterior third of the iliac crest where it divides into anterior cutaneous branch that supplies the skin over the hypogastrium and a lateral cutaneous branch that supplies the skin over the gluteal region.
- The ilioinguinal nerve enters the TAP very close to the anterior superior iliac spine (ASIS). It rises through the IOM and EOM and travels in the inguinal canal. It provides sensation to the lower abdominal wall, upper thigh and pubic regions
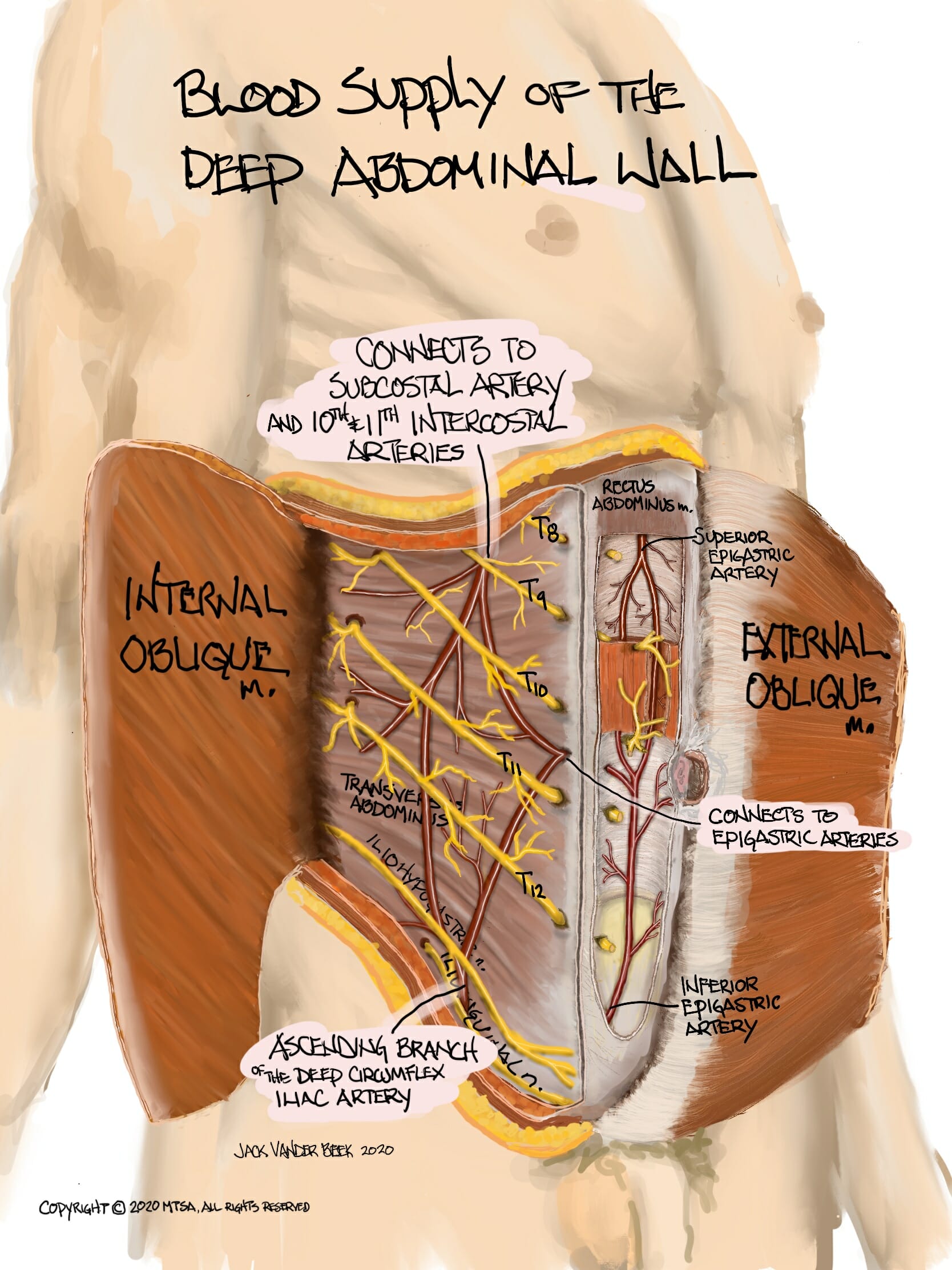
- Vasculature of the Anterior Abdominal Wall
- There is a vast network of arteries and veins within the TAP, which is responsible for the absorption of local anesthetic.
- Continuation of thoracic intercostal arteries
- Deep circumflex iliac arteries
- Superior and inferior epigastric arteries
- There is a vast network of arteries and veins within the TAP, which is responsible for the absorption of local anesthetic.
- The thoracoabdominal spinal nerves T6-T11 originate from the anterior rami of the spinal nerves and travel along their associated intercostal space, passing beneath the costal cartilage before entering the fascial plane between the TAM and IOM. They continue until they pierce the rectus abdominis muscle.
Anatomy of the Posterior Abdominal Wall
- The TFL is a series of aponeuroses and fascial layers that encapsulate the deep muscles of the back, extending from the lumbar to thoracic spine.
- The TAM and IOM taper off into the TFL
- The EOM ends in a free edge against the latissimus dorsi muscle.
- Four lumbar arteries on each side pass posterior to the psoas major and quadratus lumborum muscles, piercing the aponeurosis of the TAM and ending up in the TAP
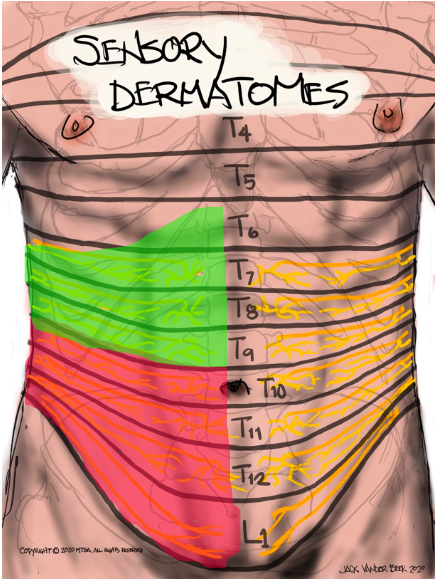
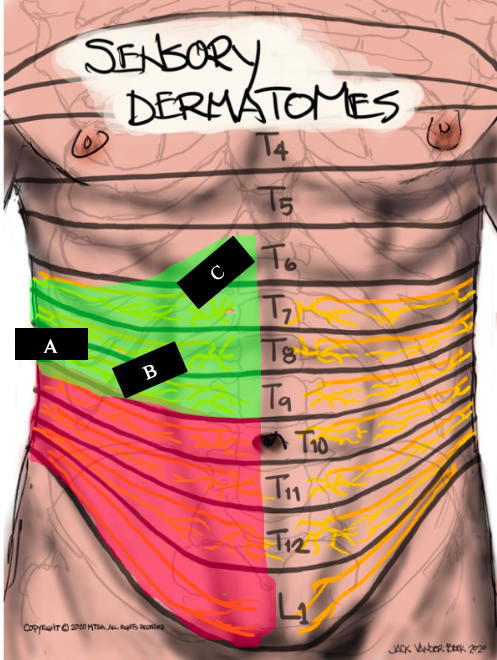
Dermatome Coverage
Dermatome coverage is dependent upon the approach (see below for the scanning technique of each)
-
- Studies demonstrate that subcostal blocks consistently result in local anesthetic spread from sub-xiphisternum (T6) to the umbilicus (T10).
- Local anesthetic spread following the lateral/posterior approach (between the iliac crest and costal margin) commonly affects T11, T12 and L1.
Dermatome mapping for the thoracolumbar spinal nerves can be captured with the following illustrations:
Scanning Techniques
Background
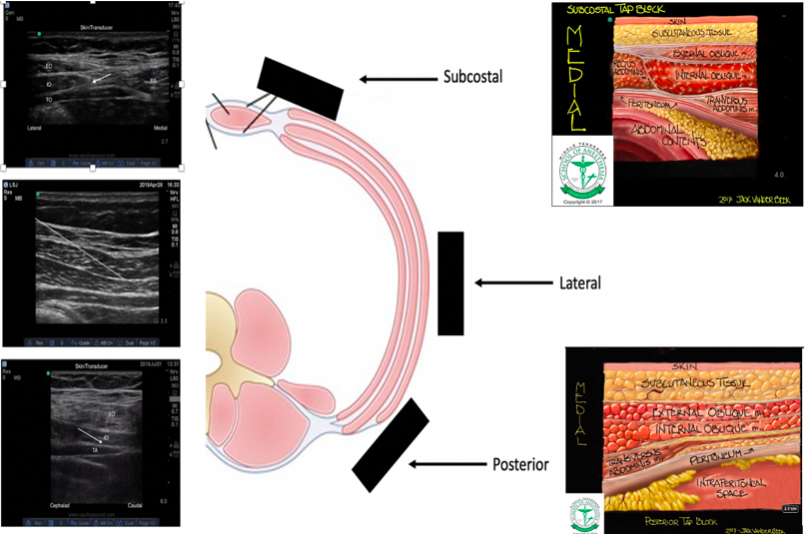
Hebbard first described the ultrasound-guided TAP block in 2007, in which the transducer oriented in transversely on the anterolateral abdominal wall where the muscle layers (EOM, IOM and TAM) are easily identifiable. After the TAP is located, the transducer is slide posterolaterally across the mid-axillary line just superior to the iliac crest. Several studies have highlighted the differences in local anesthetic spread due to complex course of the of the thoracolumbar nerves and the variations between the muscle layers and aponeurotic layers at different levels.
- In a subcostal approach, the transducer is placed lateral to the xiphoid parallel and inferior to the costal margin. The rectus abdominis, an elliptical appearing structure, is noted medially (see sonoanatomy). Scanning laterally, it abuts the linea semilunaris (LS) fascia, which is the posterior rectus sheath. The LS gives rise to the EOM, IOM and EOM.
- With a lateral approach, the transducer is placed at the mid-axillary line, superior to and parallel with the iliac crest where the EOM, IOM and TAM are identified parallel to each other (see sonoanatomy).
- When performing a posterior approach, the transducer is initially placed along the mid-axillary plane, as in the lateral approach. It is then slid posterior of the mid-axillary line until the aponeurosis of the TFL is imaged (see sonoanatomy).
Sonoanatomy
Ultrasound images and illustrations from the subcostal, lateral and posterior scanning positions with targeted local anesthetic distribution areas noted.
Needle Approach
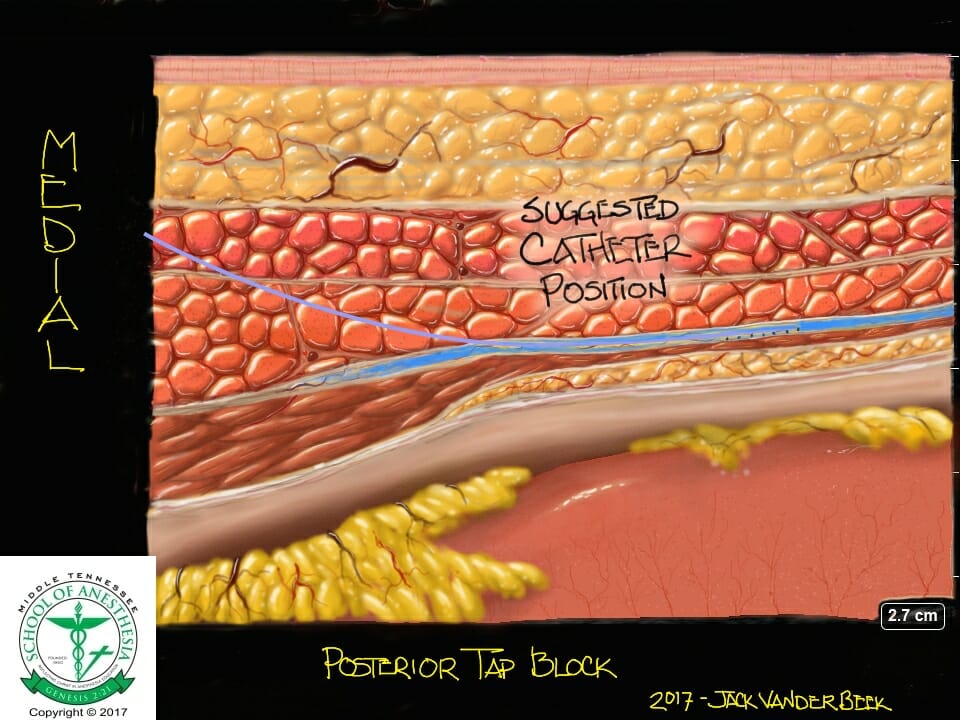
Posterior

Subcostal

In general, the needle approach is medial to lateral using an in-plane technique until the tip of the needle is visualized piercing the fascia between the IOM and TAM.
- When using the subcostal approach, the needle is inserted medial to lateral in the plane between the LS fascia (posterior rectus sheath) and superior border of the TAM (see sonoanatomy). Following negative aspiration, a small amount of local anesthetic is injected to confirm it is in the fascial plane. The needle is then slowly advanced in the space created.
- For the lateral approach the needle tip is guided posteriorly to the midaxillary line, to ensure the lateral cutaneous branches of the thoracolumbar nerves are blocked.
- The posterior approach targets the point where the IOM and TAM begin to taper off (see sonoanatomy) into the TFL.
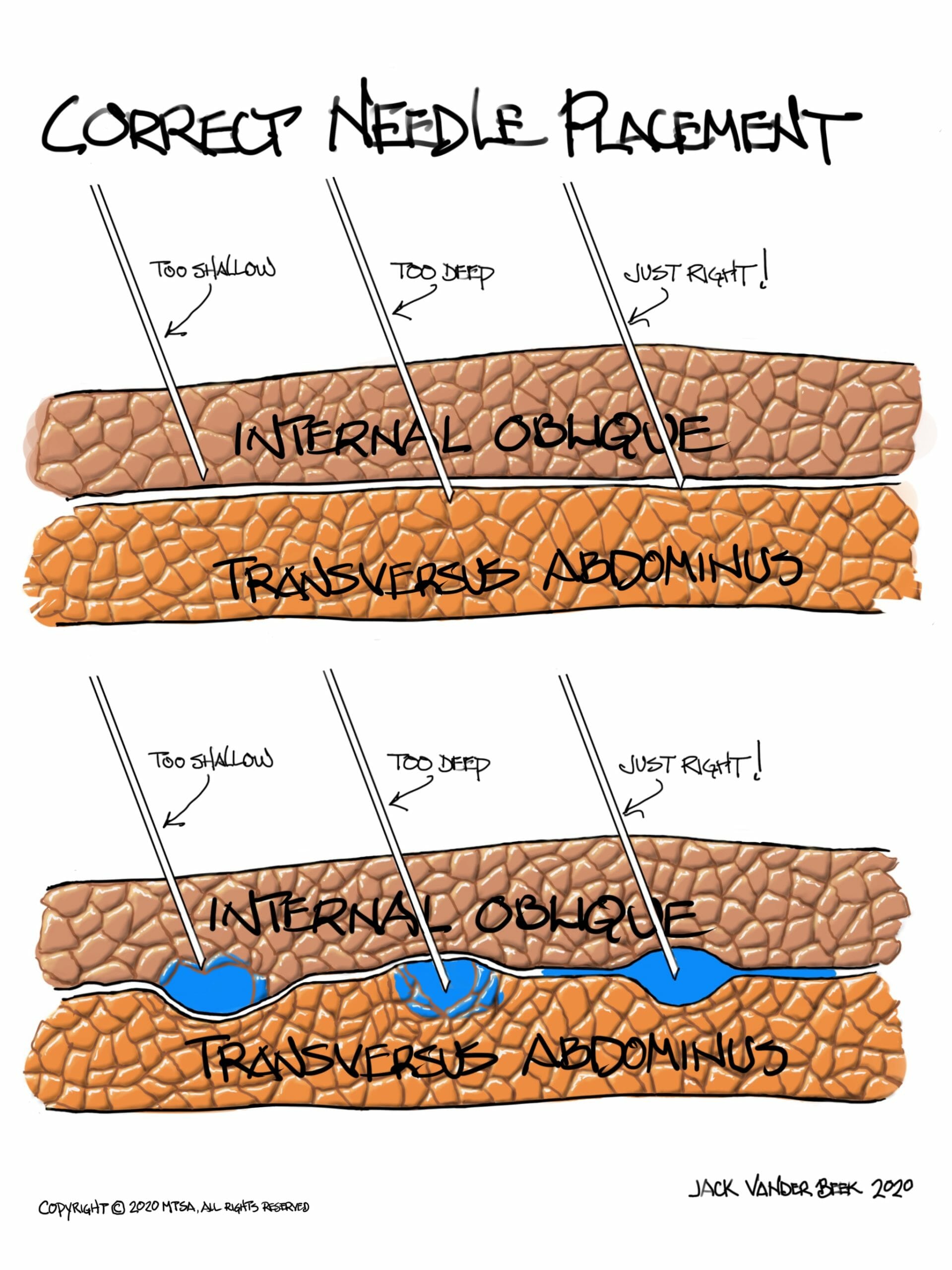
Injection Technique
- When local anesthetic is correctly injected, the fascial plane should separate in to a well-defined, hypoechoic, elliptical shape between the IOM and TAM.
-
- Injection into either the IOM or TAM will appear as a patchy opacity.
- If no injectate is noted, STOP injecting and reposition the needle. It may be in a blood vessel or the peritoneum.
-
Local Anesthetic Volume
- As a fascial plane block, large volumes of local anesthetics must be deposited to anesthetize the many small abdominal wall nerves.
- Magnetic resonance imaging and the degree of dermatomal anesthesia confirmed that the upper and lateral TAP compartments do not appear to communicate. Separate injections at the upper intercostal and lateral classic TAP plexuses are necessary to block the entire abdominal wall.
- Typically, a minimum of 20-40 mL of low concentration local anesthetic is recommended per side. This volume of local anesthetic often reaches a patient’s maximum allowable dose, especially when doing bilateral blocks. Careful dosing is required to avoid a LAST event.
- Liposomal bupivacaine (Exparel) is FDA approved for TAP blocks and can be diluted with NS to arrive at the final injectate volume.
Catheter Techniques
Bilateral subcostal and lateral catheter techniques have been described in the literature for various surgical procedures when an epidural catheter is refused or contraindicated.
- Inability to advance a catheter into the TAP indicates the needle tip has not completely penetrated the fascial plane. Slight advancement/withdrawal under ultrasound-guidance may facilitate catheter advancement.
- After placing the catheter, tip placement should be verified following removal of the needle using ultrasound to witness fluid expansion within the TAP.
- Dermabond placed at the catheter entry point can reduce backflow leakage if a catheter through the needle system is utilized.
- An infusion rate of 14 ml/hr per side of low concentration local anesthetic can be initiated to maintain the block postoperatively. Adjustments may be required if the block is insufficient in providing analgesia through the administration of routine boluses for maintaining an open fascia TAP.
Complications
- Block failure
- Local anesthetic systemic toxicity (LAST)
- Intraperitoneal injection
- Bowel injury
- Hepatic injury
- Inadvertent femoral nerve block resulting in ambulation injuries from falls in the postoperative period have been reported in the literature.
PEARLS
- Subcostal TAP blocks are indicated for surgical procedures requiring supraumbilical analgesia.
- Lateral and posterior TAP blocks provide reliable analgesia for procedures below the umbilicus.
- When performing the posterior TAP block, place ultrasound probe as posterior as possible while still imaging the 3 abdominal muscle layers to target the L1 ventral rami nerve that will often exit the TAP plane at a posterior location.
- Epinephrine additives (2.5 ug/ml) are often beneficial in extending block duration and for the early recognition of an inadvertent intravascular injections required with large volume TAP blocks.
References
- Chin KJ, McDonnell JG, Carvalho B, Sharkey A, Pawa A, Gadsden J. Essentials of Our Current Understanding: Abdominal Wall Blocks. Reg Anesth Pain Med. 2017;42(2):133‐183.
- Hebbard P, Fujiwara Y, Shibata Y, Royse C. Ultrasound-guided transversus abdominis plane (TAP) block. Anaesth Intensive Care. 2007;35(4):616‐617.
- Elsharkawy H, Bendtsen T. Ultrasound-guided transversus abdominis plane and quadratus lumborum blocks. In Hadzic A, ed. Hadzic’s Textbook of Regional Anesthesia and Acute Pain Management. New York, NY: McGraw Hill; 2017:649-649.
- Tsai HC, Yoshida T, Chuang TY, et al. Transversus Abdominis Plane Block: An Updated Review of Anatomy and Techniques. Biomed Res Int. 2017;2017:8284363.
- Milan Z, Tabor D, McConnell P, Pickering J, Kocarev M, du Feu F, Barton S. Three different approaches to the transversus abdominis plane block: a cadaveric study. Med Glas Ljek Zenicko-doboj kantona. 2011;8(2):181-184.
- Hebbard P. TAP block nomenclature. Anaesthesia. 2015;70(1):112‐113.
- Agrawal P, Farag E. Ultrasound-guided quadratus lumborum and subcostal transversus abdominis plane blocks. Techniques in Reg Anesth and Pain Management. 2014;18;163-165.
- Baker BW, Villadiego LG, Lake YN, et al. Transversus abdominis plane block with liposomal bupivacaine for pain control after cesarean delivery: a retrospective chart review. J Pain Res. 2018;11:3109‐3116.
- Seagle BL, Miller ES, Strohl AE, Hoekstra A, Shahabi S. Transversus abdominis plane block with liposomal bupivacaine compared to oral opioids alone for acute postoperative pain after laparoscopic hysterectomy for early endometrial cancer: a cost-effectiveness analysis. Gynecol Oncol Res Pract. 2017;4:12.
- Hutchins J, Vogel RI, Ghebre R, et al. Ultrasound-guided subcostal transversus abdominis plane infiltration with liposomal bupivacaine for patients undergoing robotic-assisted hysterectomy: a retrospective study. Int J Gynecol Cancer. 2015;25(5):937‐941.
- Børglum J, Jensen K, Christensen AF, et al. Distribution patterns, dermatomal anesthesia, and ropivacaine serum concentrations after bilateral dual transversus abdominis plane block. Reg Anesth Pain Med. 2012;37(3):294‐301.