Authored by:
Bill Johnson DNAP, CRNA
Director, Acute Surgical Pain Management Fellowship and Doctorate Completion Program Middle Tennessee School of Anesthesia

Overview
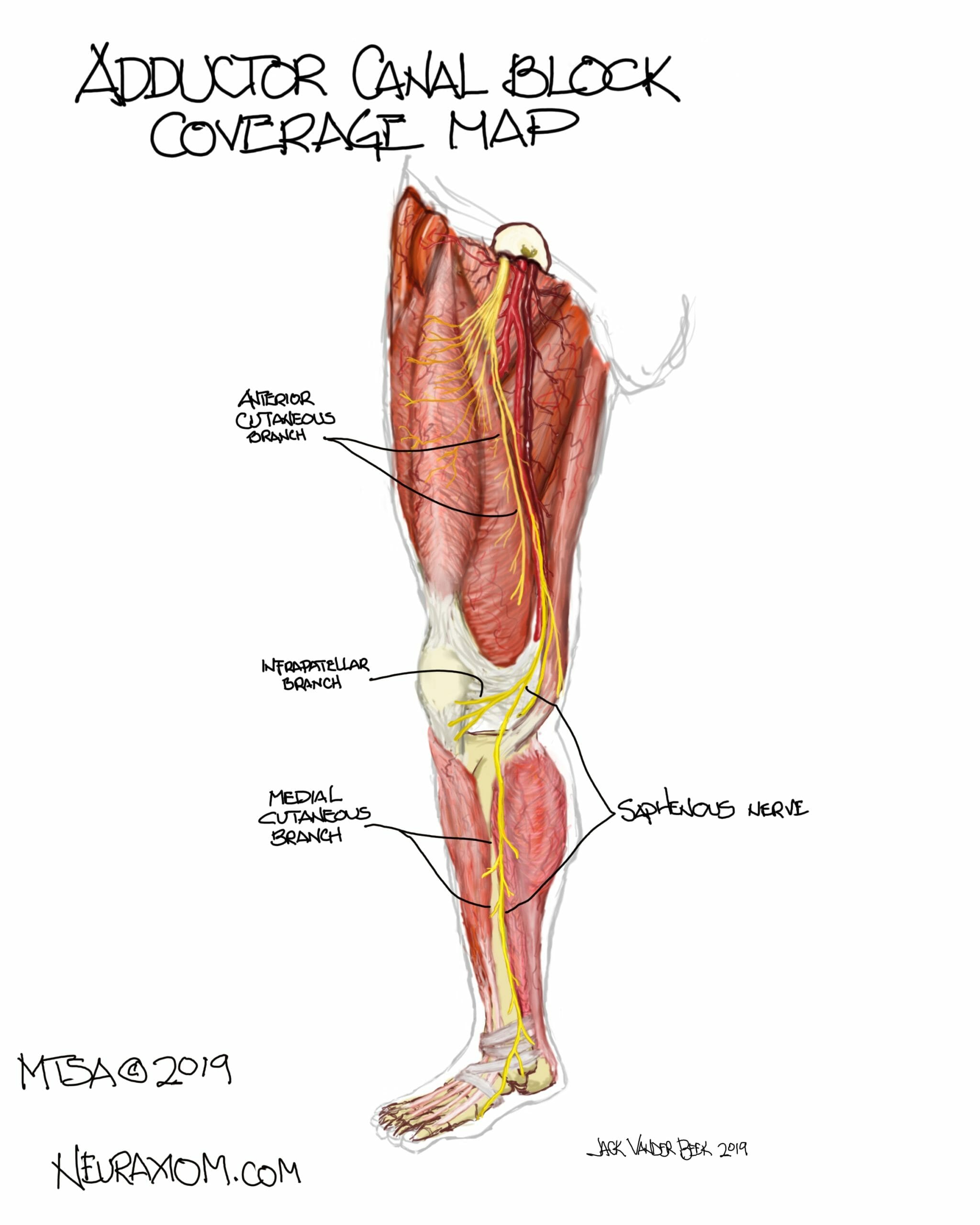
- Local anesthetic is placed within the adductor canal (AC) to anesthetize the saphenous nerve and its branches in order provide sensory analgesic coverage of the anteromedial aspects of the lower extremity from the mid-thigh area to the foot.
- A properly placed AC block can provide a quadricep muscle sparing, analgesic block of the lower extremity by avoiding proximal blockade of the femoral nerve.
Indications
Surgical indications include: Total knee arthroplasty, ACL/MCL knee repairs, patella fractures, or any surgery involving the anteromedial aspects of the lower extremity.
Positioning
Supine, with the leg slightly externally rotated.
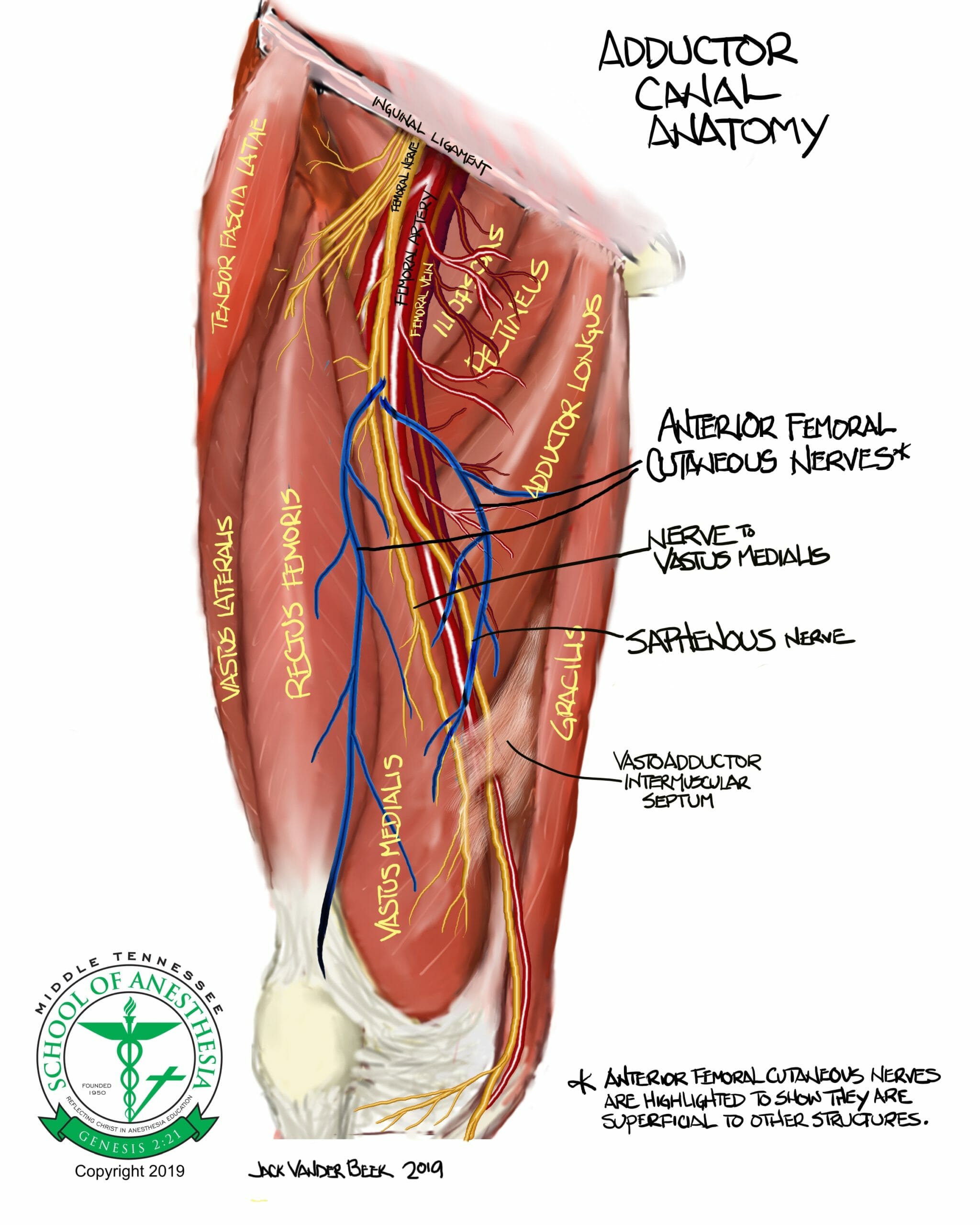
Anatomy of the Adductor Canal
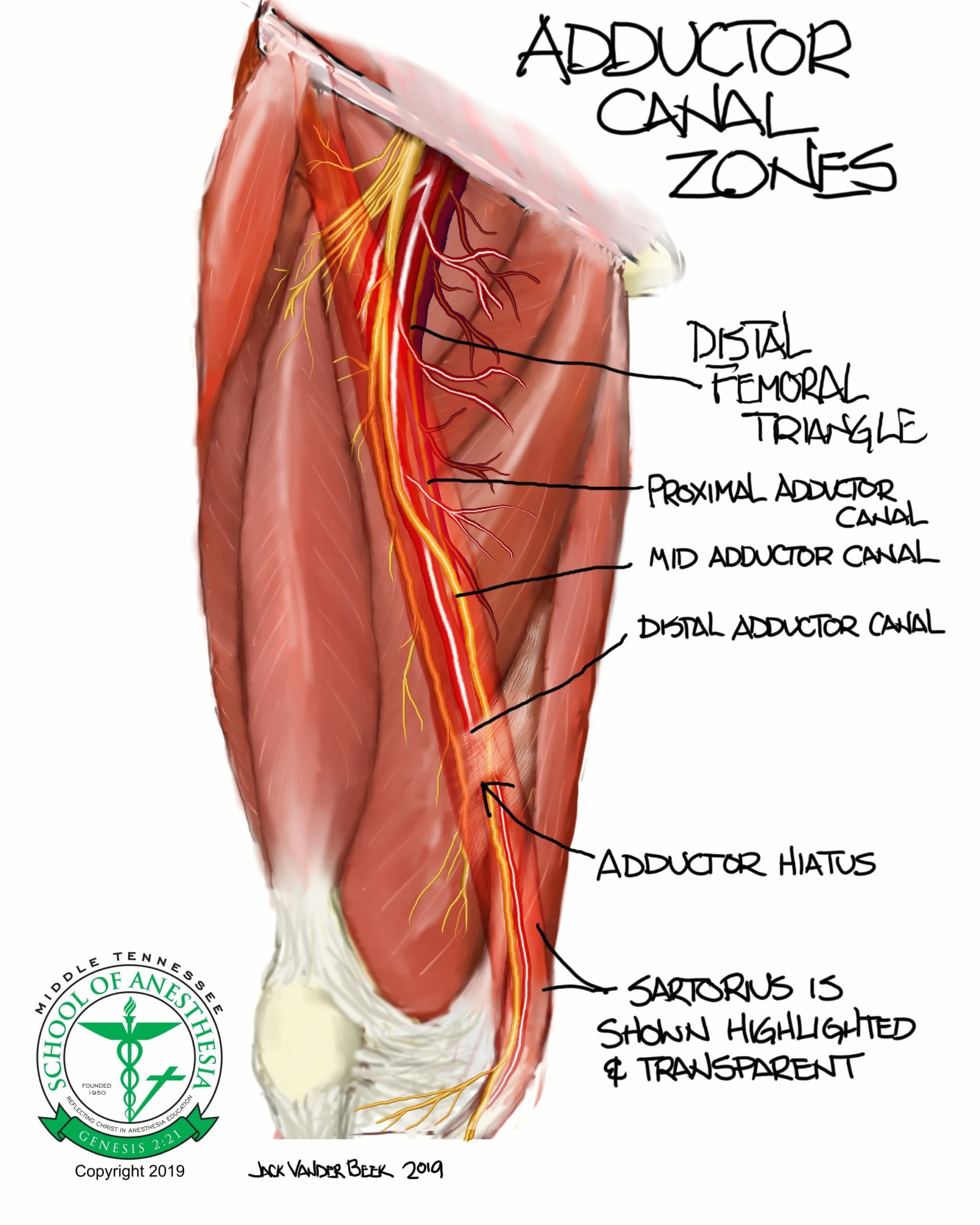
The adductor canal is a musculoaponeurotic, triangular shaped tunnel lying posterior to the sartorius muscle that begins at the distal femoral triangle (see illustration), extending distally to the adductor hiatus (a location demarcated by the point where the superficial femoral artery (SFA) exits the AC and descends posteriorly to become the popliteal artery)
Pertinent Structures located within the AC:
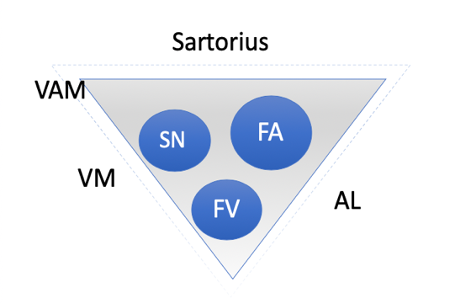
- The Vastoadductor membrane (VAM) is an anteromedial separation barrier between the vastus medialis muscle and the neurovascular structures contained with the AC. This barrier forms the “roof” of the subsartorial space and must be successfully penetrated to have a successful AC block.
- Subsartorial plexus is comprised of the saphenous nerve, anterior branch of obturator nerve, and the posterior branch of the obturator nerve.
- Saphenous nerve is a sensory-only branch derived from the femoral nerve, which originates from the L2-L4 lumbar plexus.
- The saphenous nerve enters the proximal adductor canal at the level of the distal femoral triangle and exits the AC distally at the adductor hiatus.
- Once exiting the hiatus, the saphenous nerve courses anteriorly to a more superficial location between the gracilis and vastus medialis muscles, and then travels distally in close proximity with the saphenous vein below the knee
- The saphenous nerve has 2 sensory branches which provides a significant contribution to the sensory innervation of the knee.
-
- Anterior femoral cutaneous nerve originates from the saphenous nerve just distal to the femoral triangle and gives rise to superficial terminal branches which are identified as the medial femoral cutaneous nerves. These nerves supply skin innervation to the anteromedial regions of the knee.
- The infrapatellar branch originates from the saphenous nerve as it exits the adductor hiatus. This branch innervates anteromedial aspects of the knee joint capsule and skin.
-
- Anterior branch of obturator nerve enters and merges with the saphenous nerve in the proximal region of the AC but provides innervation to the knee in only 10% of studied cadaveric specimens.
- Saphenous nerve is a sensory-only branch derived from the femoral nerve, which originates from the L2-L4 lumbar plexus.
- Posterior branch of obturator nerve enters the distal AC transiently before exiting to unite and coalesce with the posterior genicular nerves in the popliteal plexus. This nerve supplies medial and posterior sensory innervation to the knee.
- Superficial femoral artery (SFA) and vein (SFV)
-
- The SFA descends distally in the leg and travels from the medial edge of the sartorius muscle to the lateral edge of sartorius until it reaches the distal opening of the AC or the adductor hiatus before becoming the popliteal artery in the posterior knee.
-
- Medial Vastus Nerve or Nerve to the vastus medialis (NVM):
-
- This nerve is a branch of the femoral nerve that innervates the vastus medialis muscle (one of the four quadriceps muscles) and has a significant contribution to the sensory articular innervation of the anteromedial joint capsule.
- The NVM exits the femoral triangle in a self-contained sheath outside the AC distal to the femoral triangle or can be located within the AC.
- The NVM is located between the vastus medialis and sartorius muscle just distal to femoral triangle or within the body of the vastus medialis muscle depending on the distal location from the femoral triangle.
- Ultrasound identification of this nerve can be difficult in the mid-distal portions of the AC, since this nerve begins to branch in the mid-adductor canal region to innervate the vastus medialis muscle and anteromedial joint capsule.
- The medial retinacular nerve is a distal branch of the medial vastus nerve that innervates the medial retinaculum of knee joint capsule.
-
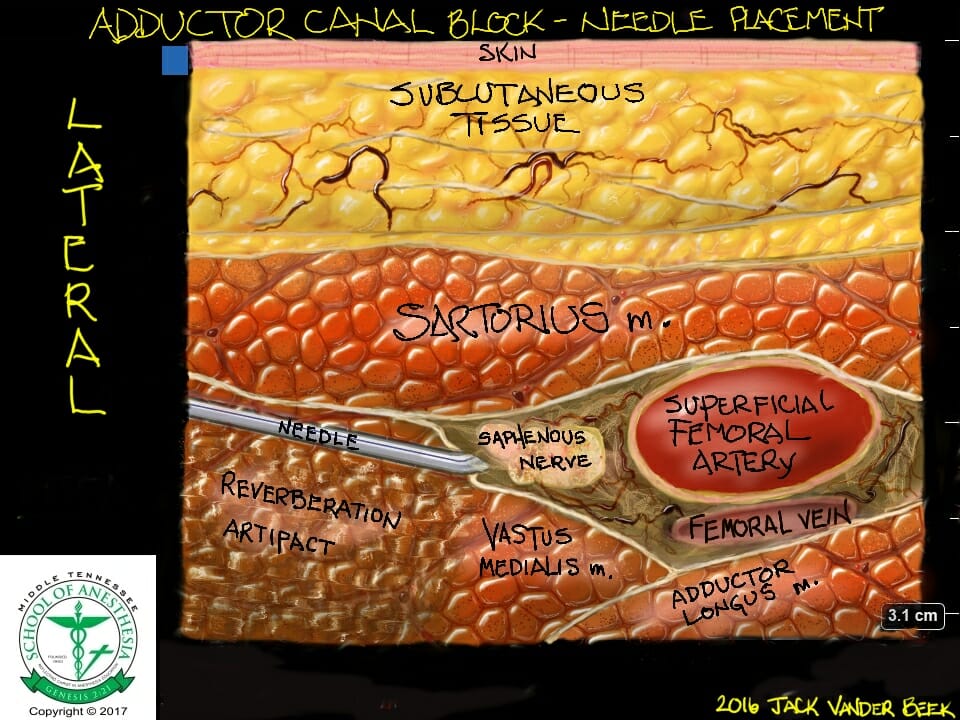
- The neurovascular structures contained in the AC are surrounded by (3) muscle groups to form the triangular-shaped AC tunnel:
-
- Vastus medialis (anterolaterally), adductor longus (posteromedially), and sartorius (superiorly)
-
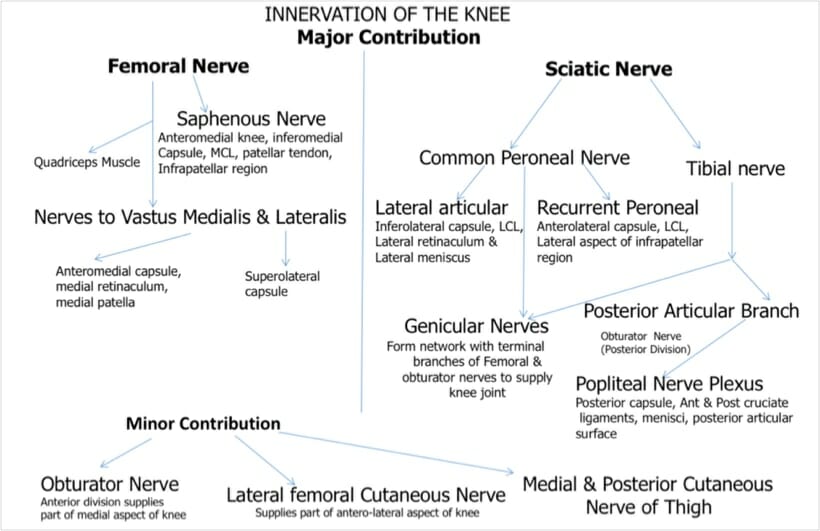
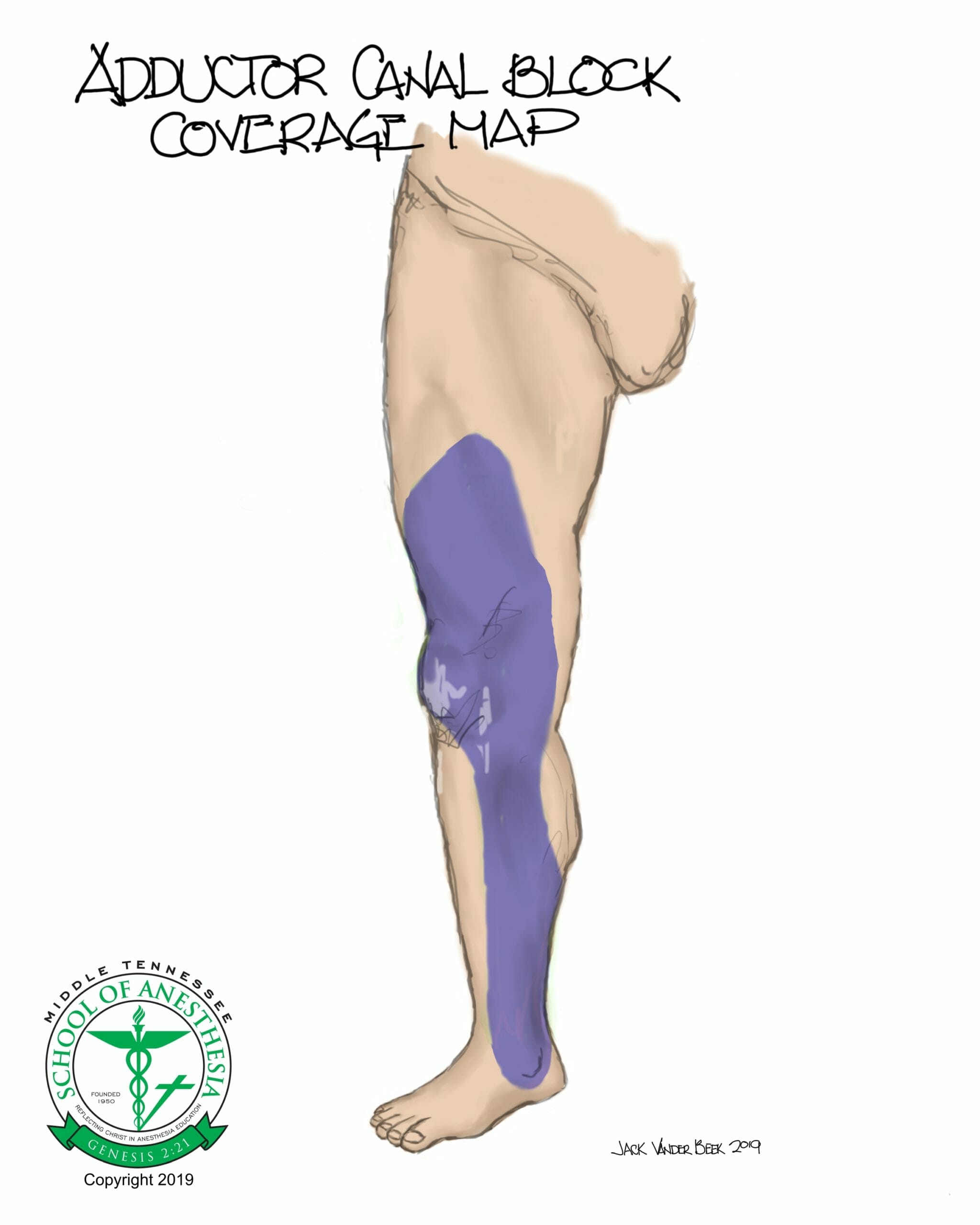
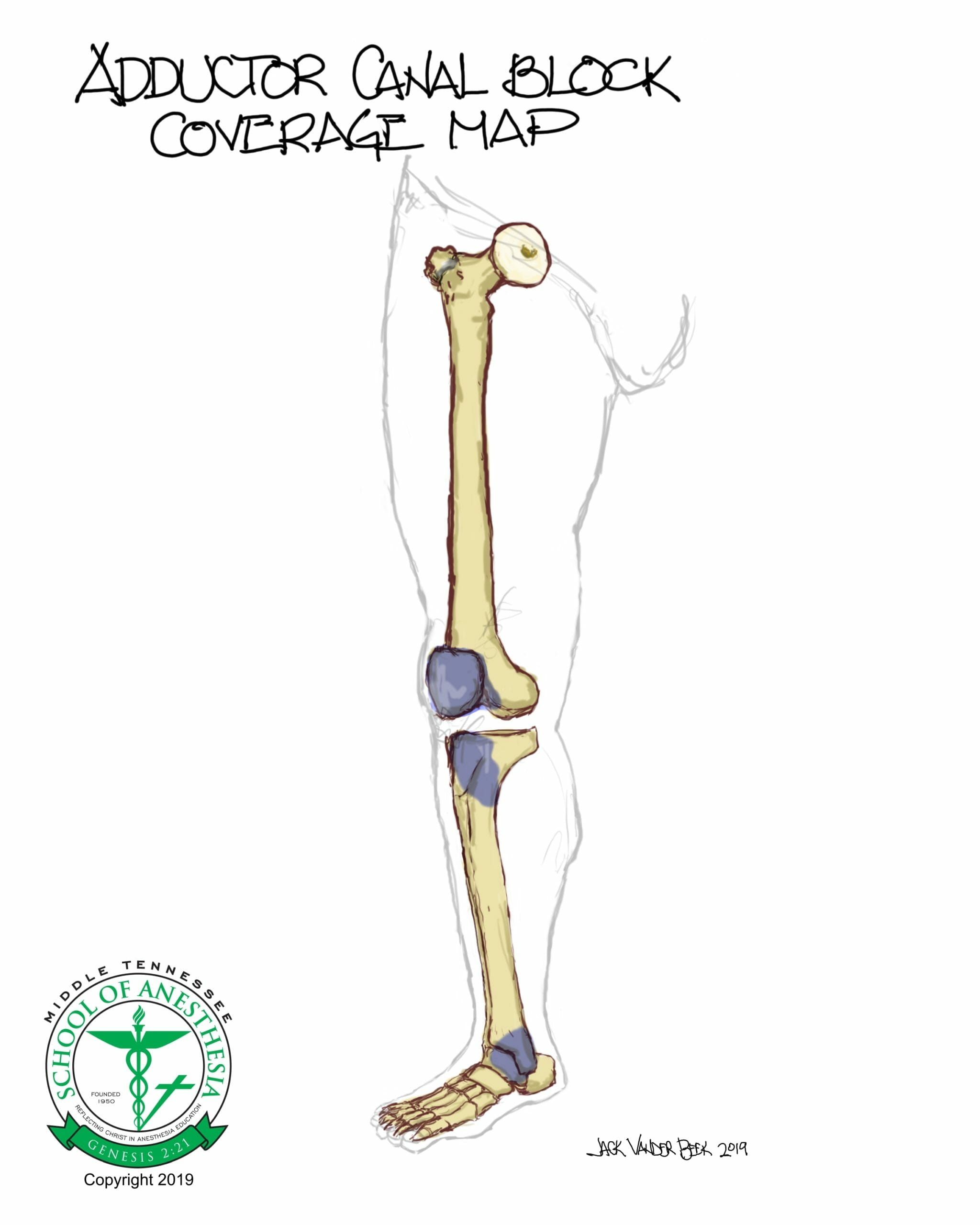
Dermatome Coverage
Dermatome mapping for the saphenous nerve and the osteotome distribution are shown in the following illustrations:
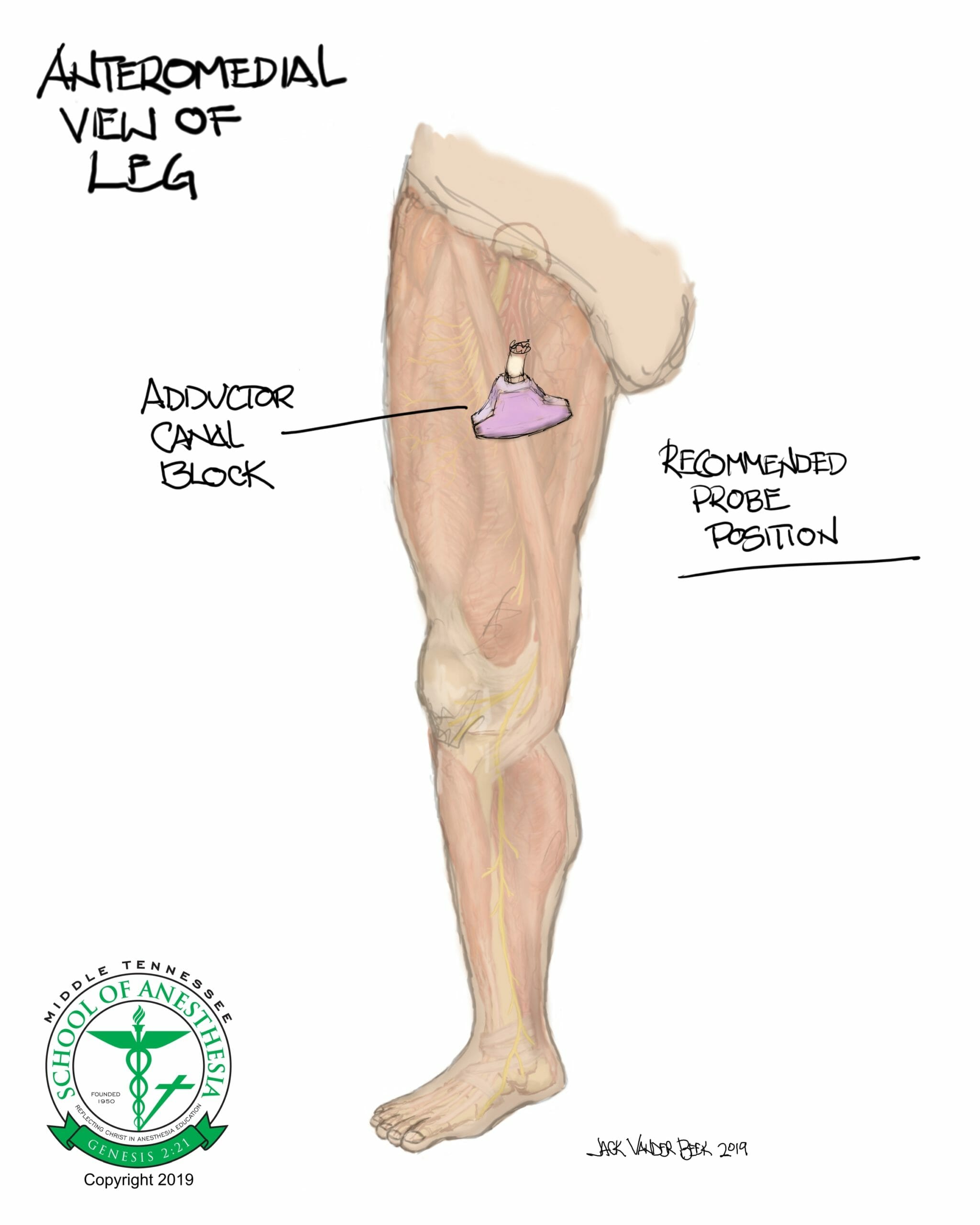
Scanning Technique
Background
Historically, local anesthetic placement within in AC was described as a midway point between the anterior superior iliac spine (ASIS) and the patella. However, cadaveric dye studies have demonstrated that blocking at this level can often corresponds to area within distal femoral triangle, leading to proximal spread and resultant quadricep weakness from a femoral nerve block. Current recommendations for identifying the ideal location for the placement of local anesthetic for the AC block is to use ultrasound and identify an area distal to the apex of the femoral triangle and within the proximal or mid AC regions.
- A high frequency linear array transducer (5-12 MHz) is used for this block. For large habitus patients or scanning depths > 4-5 cm, a low frequency 1-5 Mhz probe can facilitate proper imaging for this block.
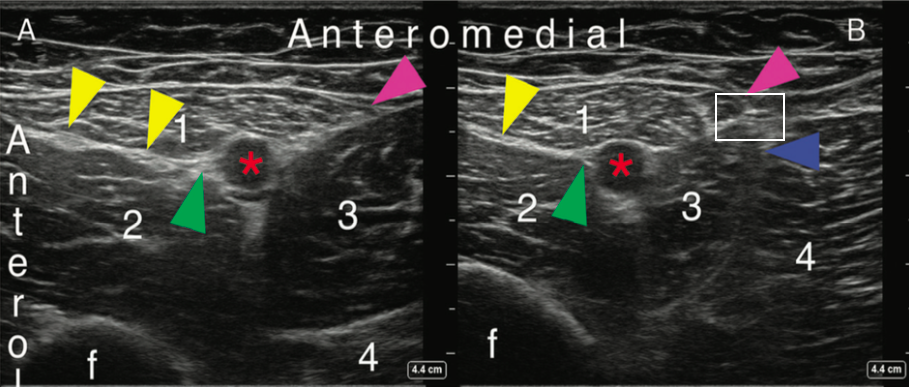
- Scanning Zones of the AC:(Side-by-side illustration of sonoanatomy and color anatomic illustrations)
- Subsartorial Femoral Block in Femoral Triangle (Figure A) is the distal portion of the apex of the FT and a location where the subsartorial plexus is formed superficially to the vastus medialis muscle. This area represents the proximal origins of the AC (Figure A) and is a midway point between the ASIS and patella when using the external landmark approach.
- Subsartorial Femoral Block in Femoral Triangle (Figure A) is the distal portion of the apex of the FT and a location where the subsartorial plexus is formed superficially to the vastus medialis muscle. This area represents the proximal origins of the AC (Figure A) and is a midway point between the ASIS and patella when using the external landmark approach.
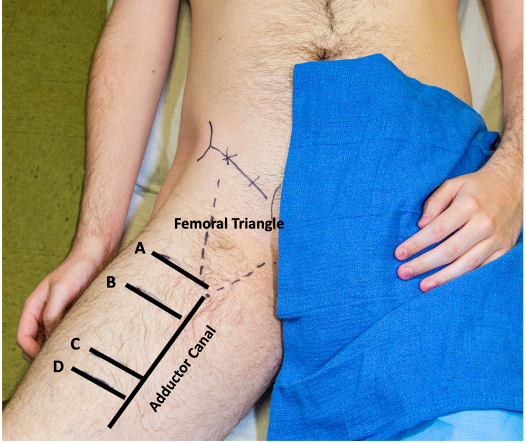
- Proximal AC (Figure B):
- Area where the saphenous nerve, SFA and SFV descend posteriorly into the AC and represents an ideal location to perform an ACB, as efficacy can be achieved with less local anesthetic.
- To identify the proximal AC with ultrasound (US), scan from the FT distally to the “intersection” of the medial borders of the sartorius and adductor longus muscle.
-
- The SFA is located inferiorly and on the medial upslope to the sartorius muscle on ultrasound, with the saphenous nerve (green arrow) being lateral from the 9-12 o’clock position relative to the SFA (Figure B). The SFV is located posterior to the SFA and is often compressed by the probe during this procedure.
- Mid-Adductor (Figure C): The SFA is located at a midway point and inferior to the sartorius muscle on ultrasound and represents an anatomical half-way point between the femoral triangle and adductor hiatus.
- Distal Adductor (Figure D): An area immediately distal to the adductor hiatus.
- Cadaveric and clinical studies have demonstrated that a block done in this region may result in a failure to anesthetize proximal sensory branches of subsartorial plexus and vastus medialis nerve.
- The saphenous nerve (green arrow) ascend superficial and exits the AC region where it lies between the sartorius (1) and gracilis (5) muscles in Figure D.
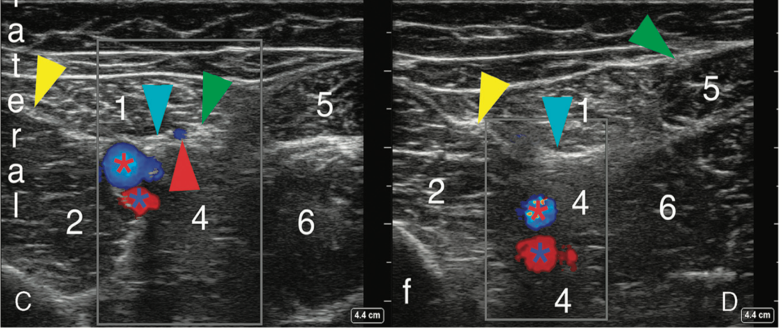
Sonoanatomy
Ultrasound images and illustration taken from the proximal AC region with noted local anesthetic targeted distribution areas.
Needle Approach
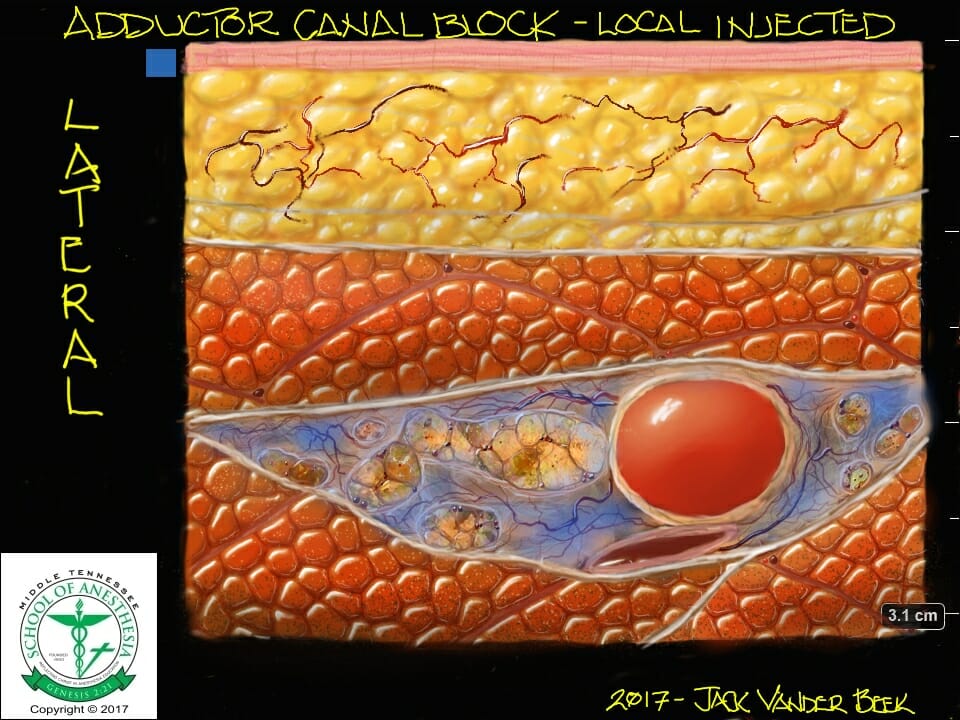
- Needle approach is from lateral-to-medial with required penetration of the needle tip through the posterior sheath of the sartorius muscle and vastoadductor membrane (“roof” of the subsartorial space).

Injection Techniques
- A distinctive “pop” is felt when the needle pierces the AC. Inject normal saline to observe anterior elevation of the vastoadductor membrane and sartorius muscle while witnessing anechoic spread of fluid over the superior aspect of the SFA. Once proper location is confirmed, continue to inject local anesthetic (15-20 ml) observing expansional spread of the subsartorial space.
- A small aliquot (5-7 ml) of local anesthetic is injected in and around the medial vastus nerve which lies lateral between the sartorius and vastus medialis muscle.
- The medialis vastus nerve is often contained within in its own fascial sheath between the sartorius and vastus medialis muscle. Blockade of this nerve as a distinctive block, has demonstrated enhanced analgesic coverage of the knee joint.
Local Anesthetic Volume
- Adductor Canal: 15-20 ml
- Vastus Medialis nerve: 5-7 ml
Catheter Techniques
- Rotating the transducer slightly to create an oblique orientation can facilitate can help facilitate catheter placement into the adductor canal region.
- Inability to advance a catheter into the AC indicates the needle tip has not completely penetrated the vastoadductor membrane or the needle is abutting against structures within the canal. A change in needle direction/angle or slight advancement under ultrasound guidance can alleviate the obstruction and facilitate catheter advancement.
- Catheters should be advanced under ultrasound guidance NO further than 3 cm into the canal.
- Ultrasound verification of the catheter tip (above or adjacent to the SFA) is accomplished with visualization of fluid or air expansion in the AC.
- Dermabond placed at the catheter entry point can reduce backflow leakage if a catheter through the needle system is utilized.
- An infusion rate of 6-8 ml/hr of analgesic strength local anesthetic can be initiated to maintain the block postoperatively. The infusion rate is adjusted as needed for insufficient analgesia or if an unexpected femoral block occurs with prolonged infusions.
Complications
- LAST (Local Anesthetic Toxicity)
- Infection
- Hematoma
- Nerve injury
- Femoral nerve block with resulting quadricep weakness
PEARLS
- Needle insertion parallel to the transducer enhances tip visualization when entering the AC to reduce saphenous nerve injury. This is best accomplished by inserting the needle several centimeters lateral to the transducer.
- Elevation of the posterior sartorius sheath and vastoadductor membrane with visualization of anechoic spread of fluid, superior and lateral to the SFA, during injection is of paramount importance. An injection of local anesthetic between these two structures or outside the AC region could result in a block failure.
- A pre-procedure scan identifying the NVM with a separate, targeted injection can improve the quality of the AC block with minimal reduction in quad strength.
- A nerve stimulator can be used by setting the pulse duration to 1 mS and an amperage of 1 mV. The patient will describe a tingling sensation on the medial aspect of their calf when the needle tip approaches the saphenous nerve.
References
- Burckett-St.Laurant D, Peng P, Giron Arango L, Niazi AU, Chan V, Agur A, Perlas A. The nerve of the adductor canal and the innervation of the knee: An anatomic study. Reg Anesth Pain Med. 2016;41(3):321-327.
- Bendtsen TF, Moriggl B, Chan V, Pedersen EM, Børglum J (2014) Defining adductor canal block. Reg Anesth Pain Med 39(3):253– 254. https://doi.org/10.1097/AAP.0000000000000052
- Bendtsen TF, Moriggl B, Chan V, Børglum J. Basic topography of the saphenous nerve in the femoral triangle and the adductor canal. Reg Anesth Pain Med. 2015;40:391–392.
- Bendtsen TF, Moriggl B, Chan V, Børglum J. The optimal analgesic block for total knee arthroplasty. Reg Anesth Pain Med. 2016;41(6):1-9.
- Kendir S, Bilge Ipek Torun, Akkaya T, Comert A, Tuccar E, Tekdemir I. Re-defining the anatomical structures for blocking the nerves in adductor canal and sciatic nerve through the same injection site: An anatomical study.
- Hadzic A, ed. Hadzic’s Textbook of Regional Anesthesia and Acute Pain Management. 2nd New York, NY; McGraw Hill Education, 2017.