Authored by:
Bill Johnson, DNAP, CRNA
Director, Acute Surgical Pain Management Fellowship and Doctorate Completion Program Middle Tennessee School of Anesthesia

Overview
This block has been considered a “spinal” of the upper extremity.
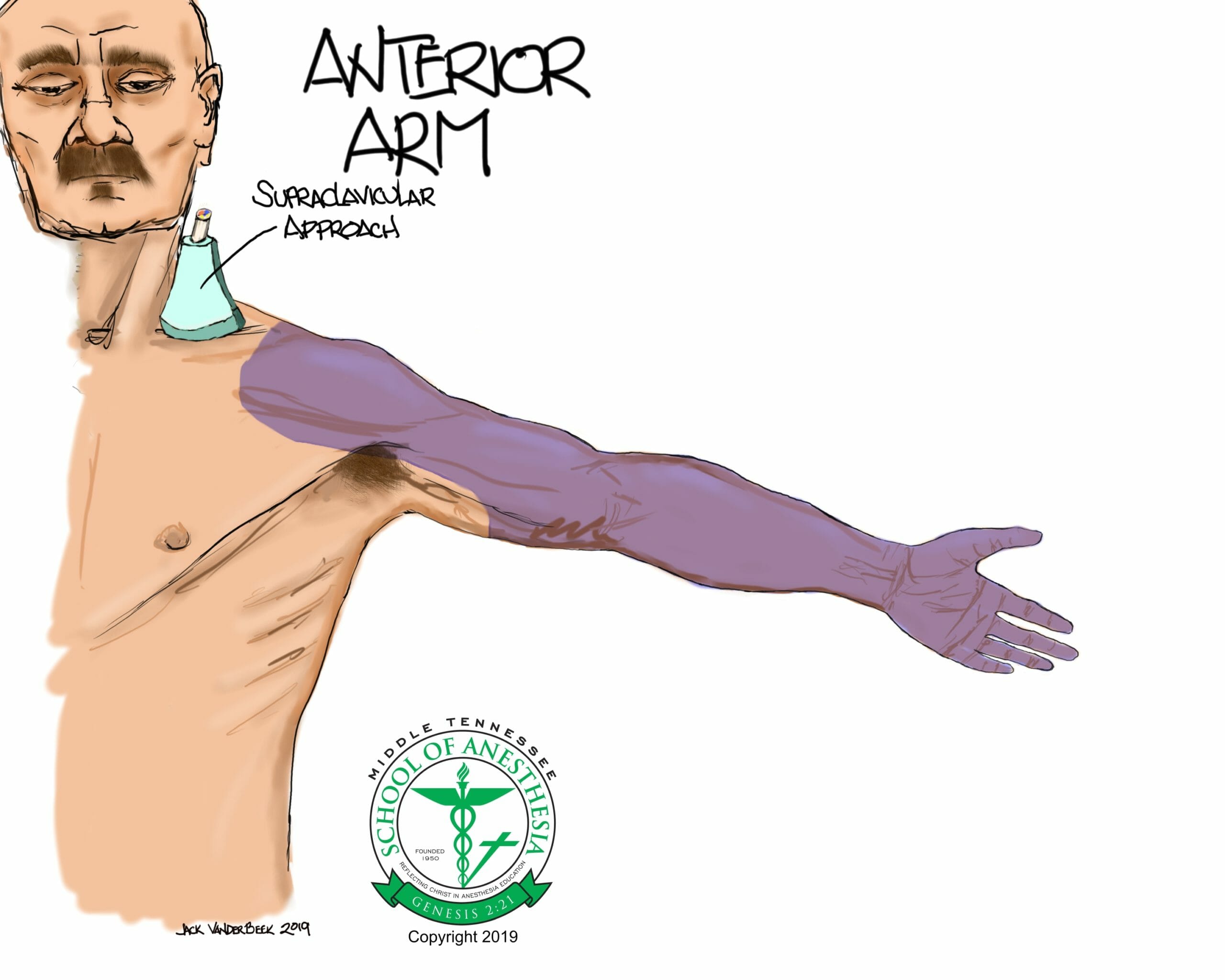
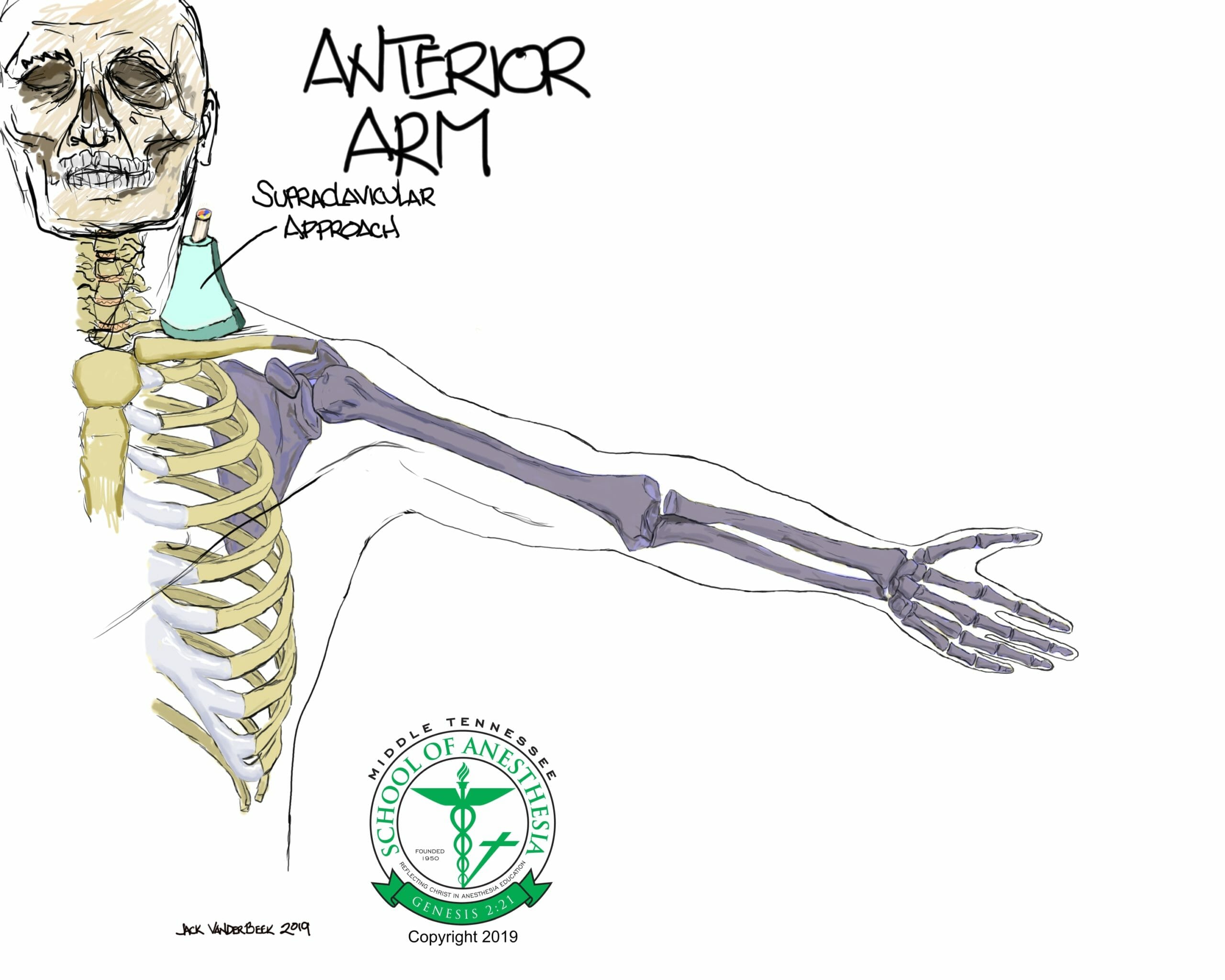
The supraclavicular regional block anesthetizes the trunks and divisions of the brachial plexus, resulting in analgesia or surgical anesthesia of the entire upper extremity with the exception of the superficial, upper medial portion of the arm which is supplied by the intercostobrachial nerve that is derived from the T2 ventral rami nerve.
Motor blockade of the upper extremity will require that a patient utilizes a support sling to minimize injury until the regional block resolves.
Indications
Surgical indications include: Any surgery involving the upper extremity.
Positioning
Supine with the head of bed elevated 30 degrees and the head turned in a contralateral direction from the block side.
Anatomy
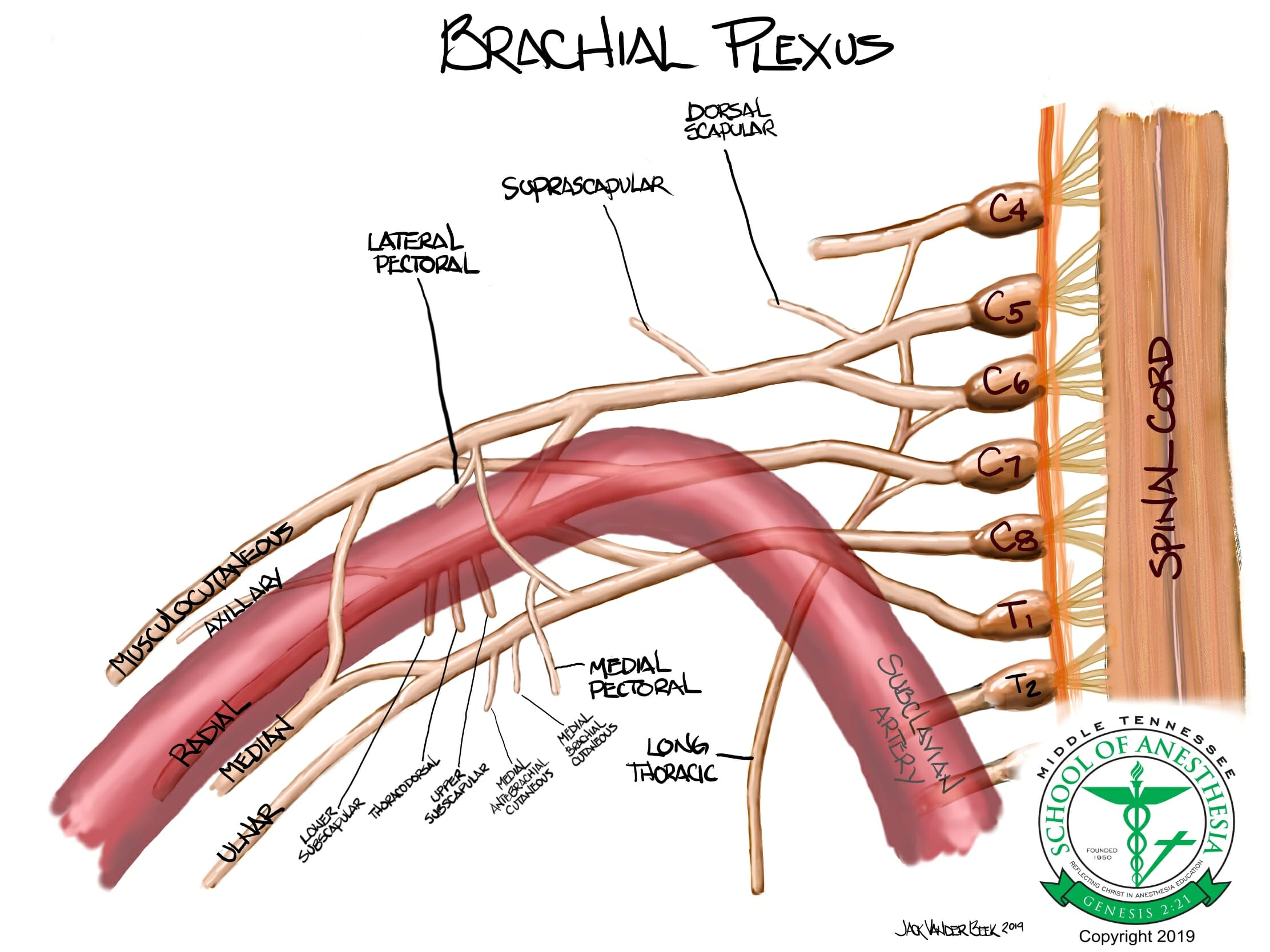
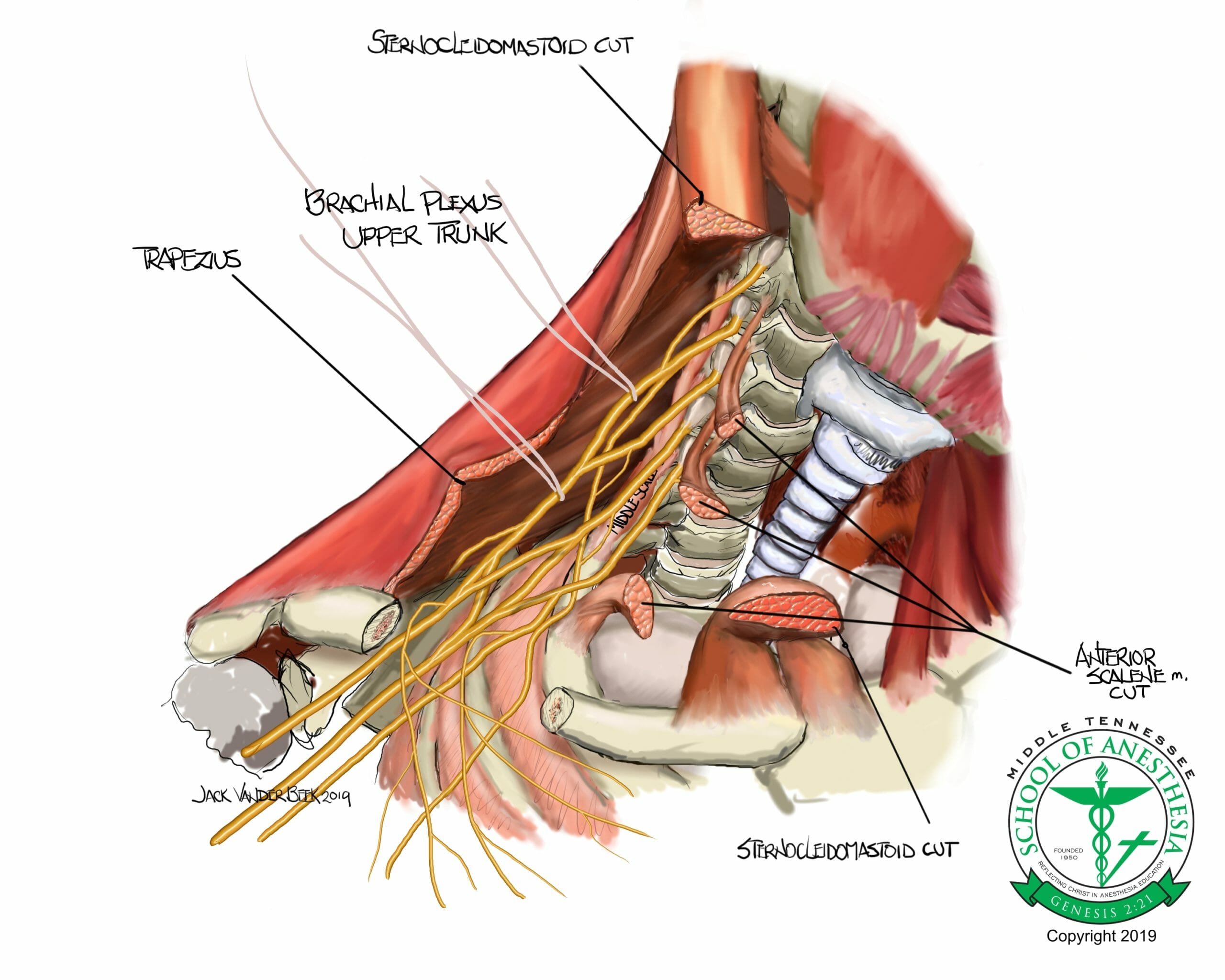
- The brachial plexus is derived from the C5-T1 cervical roots that coalesce in three primary trunks (upper, middle, and inferior). As the brachial plexus travels further distally, trunks begin to branch into divisions.
- The inferior trunk is comprised of the C8 and T1 roots which travel posteriorly between the subclavian artery and 1st rib and often times are located within a separate and distinct brachial plexus sheath than the upper and middle trunks with their associated divisions.
- The supraclavicular block is placed in area superior and parallel with the clavicle to anesthetize the trunks and divisions of the brachial plexus.
- At this level, the brachial plexus is located superior and lateral to the subclavian artery.
- This block provides anesthesia for the cutaneous distribution of the shoulder (Axillary nerve), but the internal capsule of the shoulder joint is “spared” with the Supraclavicular block.
- Fails to anesthetize the dorsal scapular and suprascapular nerves that originate from the C4-C5 brachial plexus roots/superior trunk which innervate the internal capsule of the shoulder.
- The nerves innervating the shoulder are located too cephalad in the brachial plexus region to be anesthetized with a block performed in the supraclavicular fossa region.
Dermatome Coverage
Surface Landmarks

Scanning Technique
Place the probe parallel and above the distal portion of the clavicle. Begin sliding the probe medially in a parallel and superior fashion to the clavicle until the subclavian artery comes into view. Tilting the probe can improve the visualization of the brachial plexus which is superior and lateral to the subclavian artery.
Sonoanatomy
Needle Approach
The needle should be directed in a lateral-to-medial direction using an in-plane approach. In order to prevent a neural injury or pneumothorax with this block, initially insert the needle at an extremely shallow depth to obtain good ultrasound needle visualization of tip before advancing towards the brachial plexus. Starting with a shallow needle approach will also help avoid an inadvertent puncture of the pleura, which is often times located only 2-3 cm below the skin.
A distinctive neural sheath “pop” will often be sensed when the needle tip is advanced into the brachial plexus sheath. Once this “pop” is felt, there is no need to advance the needle any further into the brachial plexus for adequate spread of local anesthetic.
Nerve Stimulator Guidance
Flexion or extension of the wrist, external or internal rotation of the wrist, movement of fingers, flexion of the elbow are all twitch responses of terminal nerves of the brachial plexus. The elicitation of these twitches at 0.3-0.5 mA range and loss of these twitch responses at 0.2 mA indicate a proper location of the needle tip within the brachial plexus neural sheath.
Injection Technique
After negative aspiration for blood, local anesthetic should be slowly injected in small aliquots volumes (3-5 ml) inside the perineural sheath which surrounds the brachial plexus at a lateral and superior location relative to the subclavian artery.
An additional “corner pocket” injection of local anesthetic should be completed at a location that is inferior and lateral to subclavian lateral in order to target the inferior trunk which can often be located outside the brachial plexus perineural sheath.
Local Anesthetic Volume
Supraclavicular: 12-15 ml
“Corner Pocket”: 5 ml
Catheter Techniques
- A catheter can be placed 2-3 cm within the perineural sheath to provide prolong coverage with a continuous infusion.
- “Dry” catheter techniques are often requested by the surgeon, in which, the catheter is initially placed preoperatively using Saline to expand the space for catheter placement and then dosed postoperatively when the surgeon has had to opportunity to perform a neuromuscular assessment of the extremity. Once assessment has been completed for a potential intraoperative nerve injury, the catheter can be bolused and infusion started for a postoperative analgesic benefit.
- Due to shallow location of this block, catheter migration and backflow leakage can be a common occurrence when catheters are placed in the supraclavicular fossa. Using self-coiling catheters and Dermabond may help minimize these catheter placement failures.
- Infusion rates can be initiated at 4-6 ml/ hour.
PEARLS
- A successful “corner pocket” injection can be performed by using the 1st rib as a “backstop” while performing an injection lateral and inferior to the subclavian artery to target the inferior trunk region of the brachial plexus. If an injection in the “corner pocket” is performed first, this creates a slight elevation of the entire brachial plexus facilitating further injections into rest of the brachial plexus. Failing to inject the “corner pocket” can result in nerve sparing of the ulnar distribution of the upper extremity.
- The suprascapular nerve (SSN) can often be located and avoided with the ultrasound view of supraclavicular block. As the suprascapular branches off the superior trunk, it descends and travels beneath the omohyoid muscles before existing posteriorly to innervate the shoulder joint. On ultrasound, the SSN can be found lateral to brachial plexus and posterior to the omohyoid muscles. The use of a nerve stimulator during the performance of this block can assist in avoiding the SSN, as external rotation and slight abduction of the upper arm will be elicited as a muscles twitch response when the needle tip is in close proximity to the SSN.
- Use color Doppler to rule out the presence of aberrant vessels in Supraclavicular region:
- Suprascapular, dorsal scapular, or transverse cervical arteries are aberrant vessels that are often appear in this area and can be unrecognized or indistinguishable from the omohyoid and/or serratus anterior muscle groups. Performing a Doppler scan in the area of the needle path area before needling can help to distinguish these aberrant vessels from other structures in the area.
- If these vessels are present, move the probe to a more cephalad location to avoid these vascular aberrant structures.
- Avoid direct nerve contact with needle tip by halting the advancement of the needle once a distinct “pop” is sensed. There is no need to advance the needle in between the trunks and division when distributing local anesthetic for this block.
- Always Identify the 1st rib and pleura before needling begins at a an extremely SHALLOW needling angle to avoid a pneumothorax.
- Often times, the clavicle itself will be an obstacle for an in-plane needling approach. This needling obstruction from the clavicle can be improved by slightly rotating probe away from the clavicle or moving the probe more cephalad while maintaining a good ultrasound view of the brachial plexus. These probe maneuvers will provide more needling space and better needle-to-probe alignment when performing this block.
- The ultrasound probe should be as perpendicular to skin as possible to avoid excessive “tilting” of the probe in obtaining an ultrasound view of the brachial plexus. This excessive tilt can impair in-plane needle visualization during needling.
- Excessive “tilting” can be avoided by moving the probe more cephalad or rotating the probe away from the clavicle to improve the perpendicular orientation of the probe with the skin.
References
- Supraclavicular blocks. In Peripheral Nerve Blocks and Anatomy for Ultrasound-Guided Regional Anesthesia, ed Hadzic A. 2nd ed. McGraw Hill Medical: New York, NY. 2012.
- Li WJ, Songthamwat B, Samy W, Sala-Branch X, Karmaker KM. Ultrasound-guided costoclavicular brachial plexus block: Sonoanatomy, technique, and block dynamics. Reg Pain and Med. 2017;42(2):233-240.
- Supraclavicular Block. American Society of Regional Anesthesia. http://www.usra.ca/regional-anesthesia/specific-blocks/upper-limb/suprablock.php. Accessed August 30, 2017.
- Mak, PH, Irwin MG, Ooi CG, Bm Chow. Incidence of diaphragmatic paralysis following supraclavicular brachial plexus block and its effect on pulmonary function. 2001;56(4):352-356.
- Petrar SD, Seltenrich ME, Head SJ, Schwarz SK. Hemidiaphragmatic paralysis following ultrasound-guided versus infraclavicular brachial plexus blockade: a randomized clinical trial. Reg Anesth Pain Med. 2015;40(2):133-138.