Authored by:
Bill Johnson DNAP, CRNA
Director, Acute Surgical Pain Management Fellowship and Doctorate Completion Program Middle Tennessee School of Anesthesia

Overview
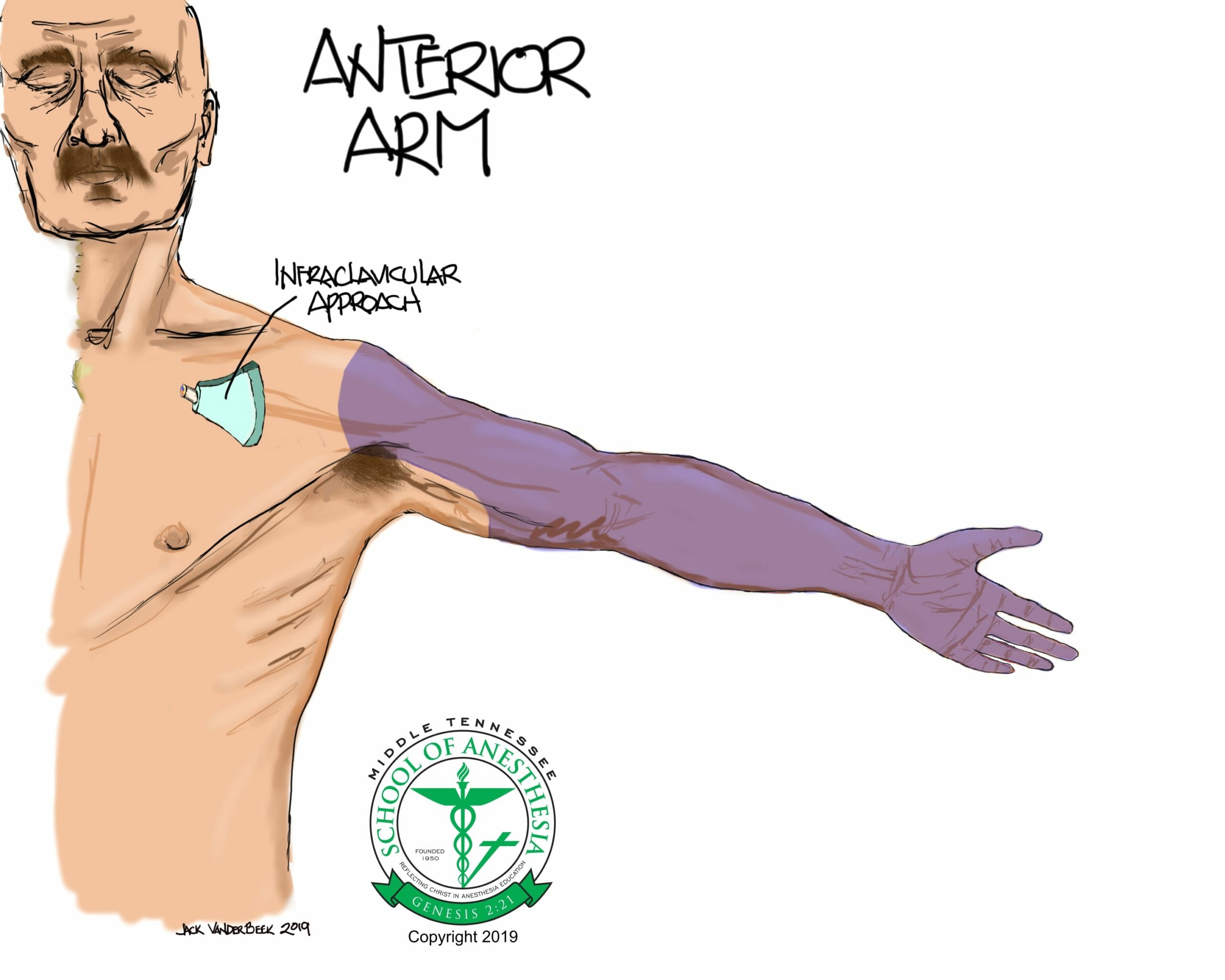
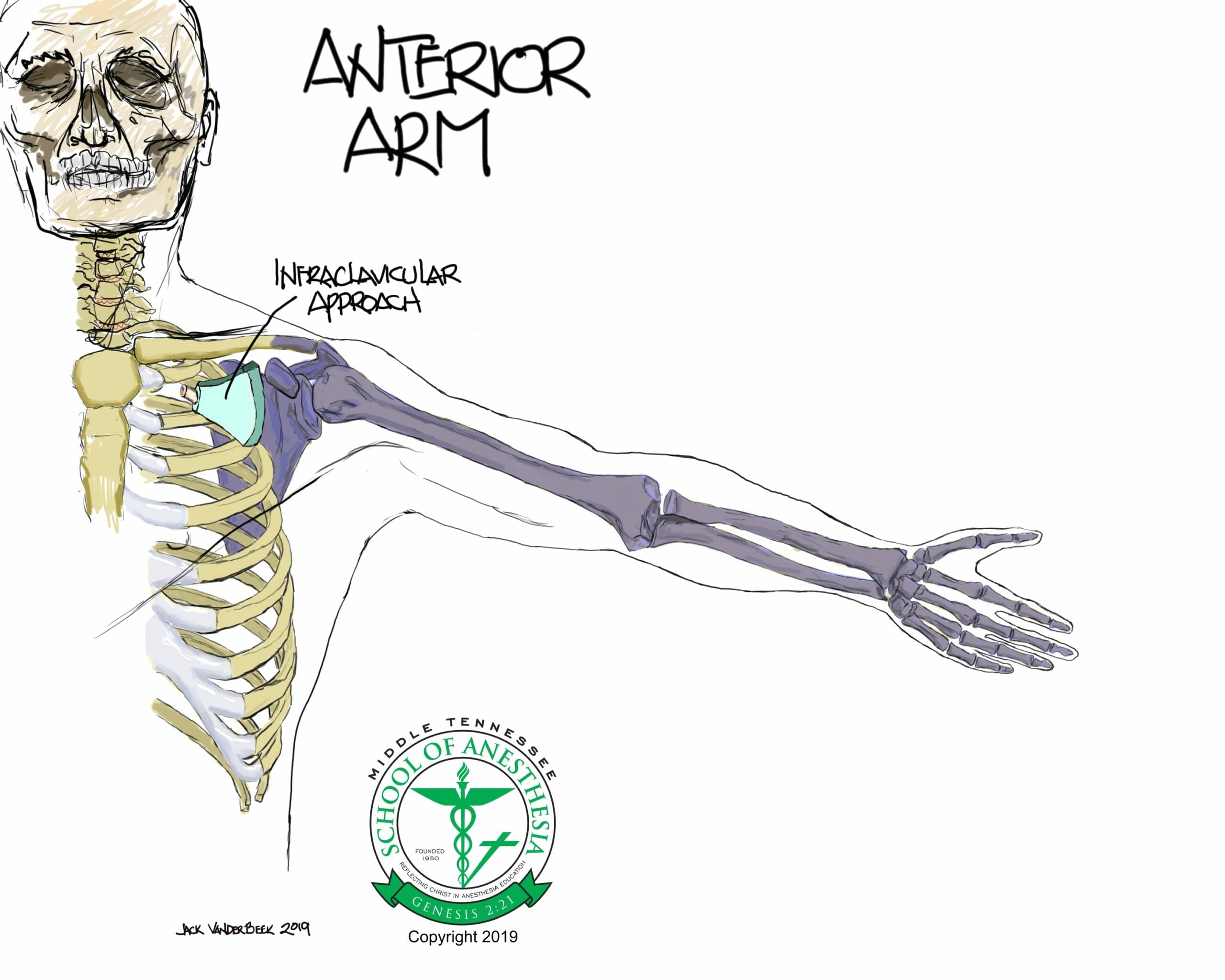
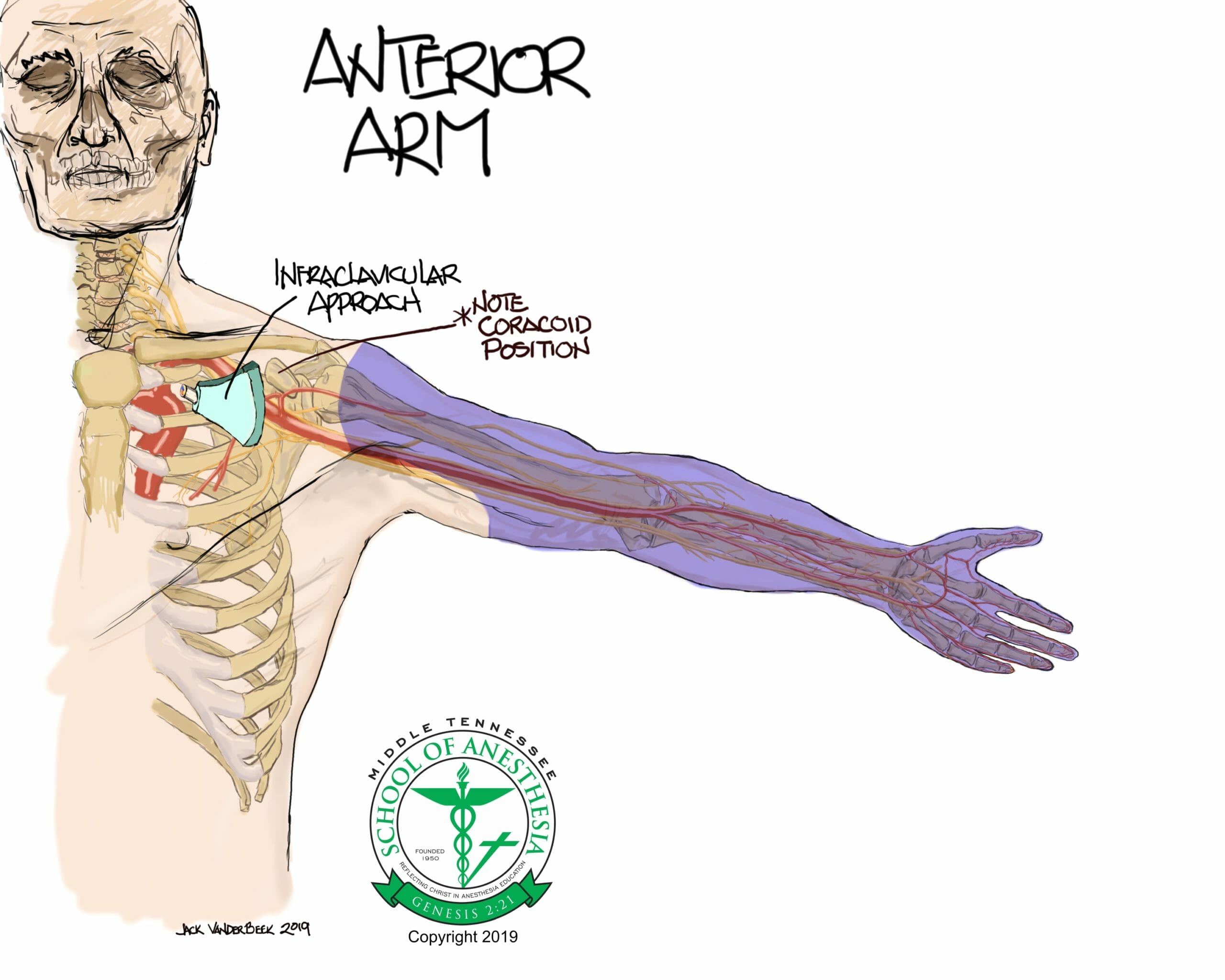
A block performed at the infraclavicular (inferior to the clavicle) levels anesthetizes the brachial plexus at the level of the cords with resultant sensory and/or motor blockade of the entire upper extremity.
Fails to adequately anesthetize the shoulder capsule by sparing blockade of the suprascapular nerve which has a more proximal take-off from the superior trunk of the brachial plexus.
Indications
Surgical indications include: Any surgery involving the upper extremity.
Positioning
Supine with the head of bed elevated 30 degrees and the head turned in a contralateral direction from the block side.
Anatomy
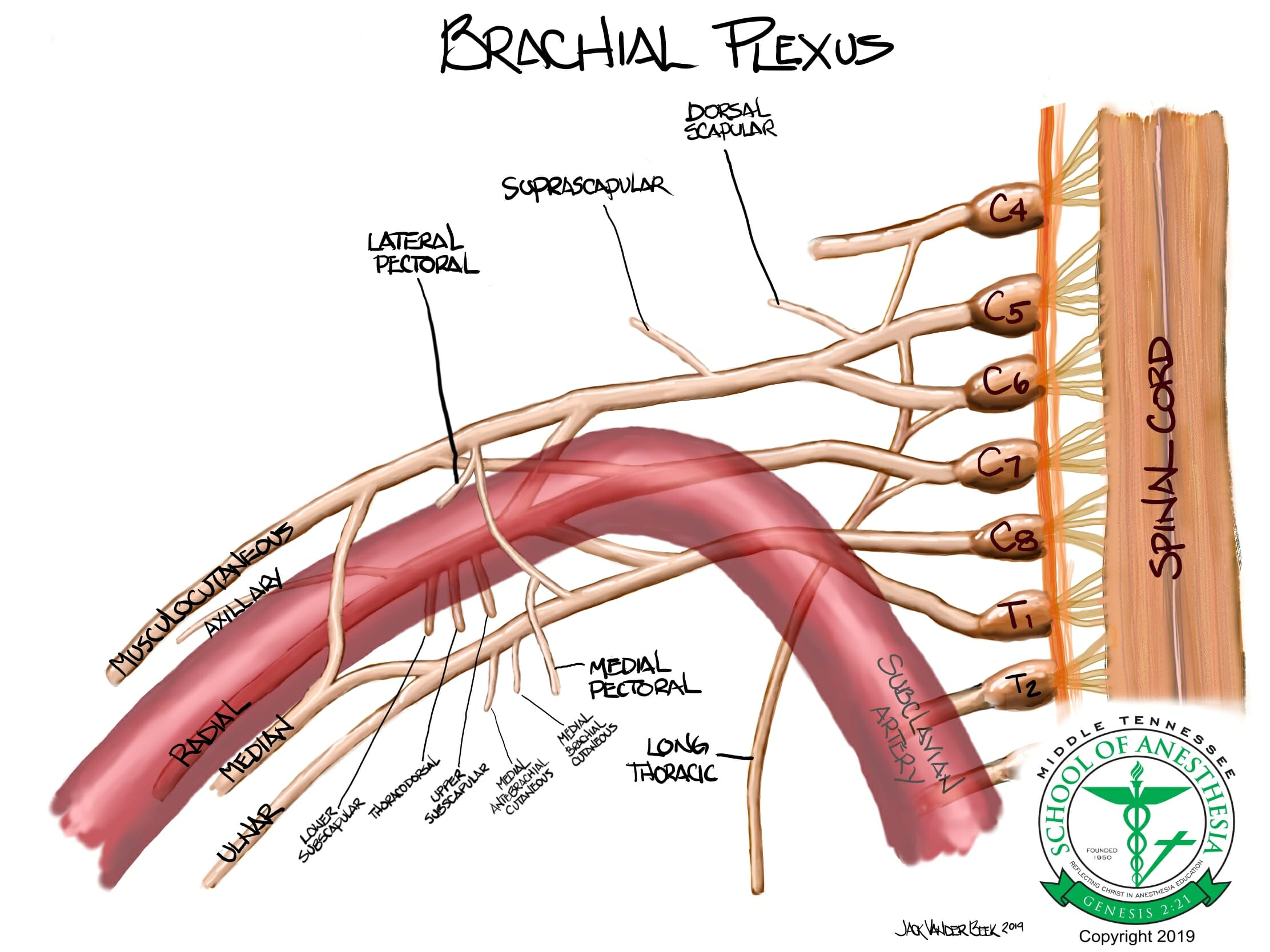
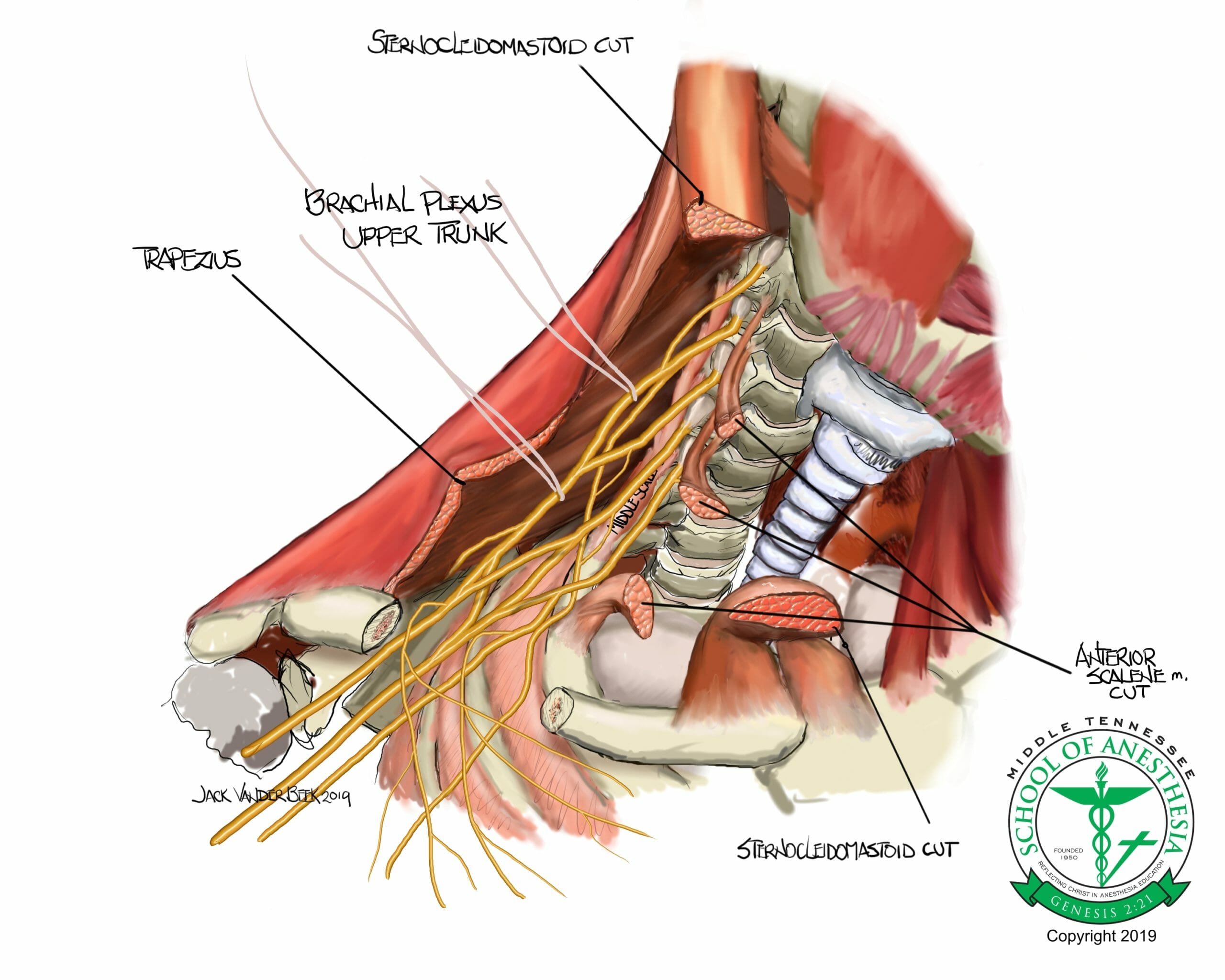
- The brachial plexus is derived from the C5-T1 cervical and thoracic roots that coalesce to form three primary trunks (upper, middle, and inferior). As the brachial plexus travels further distally, trunks begin to branch into divisions. At the level of the divisions, the brachial plexus courses under the clavicle and above the 1st rib to become the cords. The cords are located is close association relative to their anatomic location around the axillary artery and are labeled medial, lateral, and posterior cords.
- Blockade of the medial, posterior, lateral cords will anesthetize all of the brachial plexus terminal nerves (radial, medial, ulnar, median, musculocutaneous, and axillary).
Dermatome Coverage
An infraclavicular block fails to anesthetize the upper inner portion of the arm which is supplied by a sensory branch of the intercostobrachial nerve (branch of the T2 ventral rami nerve).
Surface Landmarks
Identification of the coracoid process is critical starting point for probe placement. The coracoid process is a prominent bony structure located on the medial aspect of shoulder joint. Palpitation of this structure with the arm at neutral side location should facilitate this assessment. Elevation of the arm during palpitation of this bony structure will result in the disappearance of the coracoid process which is a helpful assessment tool in evaluating the correct location of this structure.
Scanning Technique
- Begin by abducting the arm to elevate the clavicle and bring the brachial plexus to a shallower location before scanning. This maneuver is referred to as the “Houdini Clavicle” position which facilitates more needling room (2-4 cm) between the probe and clavicle.
- The brachial plexus in the infraclavicular region is located posterior to the pectoralis major and minor muscles at a depth usually greater than 3 cm. In patient with larger pectoral muscles, a deeper initial scan depth setting or use of a curve array probe may be required.
- Depth to Brachial plexus:
- 3-5 cm: 6-16 MHz high frequency, linear array probe
- > 5 cm: 2-5 MHz low frequency, curve array probe
- The probe is place in a parasagittal alignment and adjacent to the lateral aspect of the coracoid process of the shoulder.
- Identification of the axillary artery should be the primary goal, as the brachial plexus cords lie adjacent to this pulsatile structure.
- Slight tilting and the application of firm probe pressure may facilitate better visualization of the brachial cords.
- Utilize doppler color flow to properly identify any aberrant vessels in the direct needle path. The axillary vein is often located posterior and medial to the axillary artery and should be avoided during needling.
- When using the RAPTIR approach (see below), scan for the presence of the suprascapular nerve as it diverges away from the superior trunk by performing a typical interscalene block scan.
- Depth to Brachial plexus:
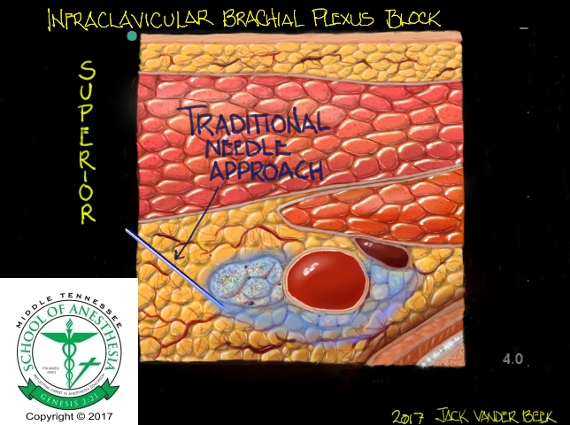
Sonoanatomy
Needle Approach
In the classic, infraclavicular approach, the needle is directed in a cephalad-to-caudad direction between the probe and clavicle. Rocking of the probe can improve needle insonization and visualization of the needle tip as the needle approaches the brachial plexus. An alternative RAPTIR (Retroclavicular Approach to the Infraclavicular Region) approach can be utilized by starting the needle in a posterior location from the clavicle. The RAPTIR approach brings the needle and probe into a more parallel position with each other facilitating better viewing of the needle tip. This approach requires the following considerations to avoid a pneumothorax:
- Slightly oblique the probe in a lateral direction so that the needle is also directed laterally away from the chest wall to avoid a pneumothorax.
- The needle should remain parallel with the bed at all times during needling.
- There is a “blind spot” that is encountered when the needle passes under the clavicle. The width of the clavicle should be measured in advance and a “stop gap” measure taken when advancing the needle to ensure proper insertion depth and visualization of the needle tip as it passes under the clavicle.
- The insertion site is determined by the overall depth to the brachial plexus in the infraclavicular region. Begin by inserting the needle posteriorly from the probe at the depth that coincides with the ultrasound depth.

Nerve Stimulator Guidance
- Flexion or extension of the wrist, external or internal rotation of the wrist, movement of fingers, flexion of the elbow are all twitch responses of terminal nerves of the brachial plexus. The elicitation of these twitches at 0.3-0.5 mA range and loss of these twitch responses at 0.2 mA indicate a proper location of the needle tip within the brachial plexus neural sheath.
- Elicitation of biceps flexion or deltoid muscle could indicate the needle tip in close proximity with musculocutaneous or axillary nerves. Both of these nerves have proximal branching from the lateral (musculocutaneous) and posterior cords (axillary) of the brachial plexus. Advancement of the needle is warranted if this twitch responses occur in order to distribute local anesthetic even around the cords of the brachial plexus.
Injection Technique
- The needle tip using the classic, infraclavicular approach will enter the brachial plexus adjacent to the lateral cord. An injection of local anesthetic at this location will facilitate a blockade of the lateral cord.
- Once the lateral cord is injected, an attempt to should be made to locate the needle tip between the axillary artery and posterior cord, or at 6 o’clock position relative to the axillary area. An injection at the location will block the lateral and medial cords with a “horseshoe” spread pattern.
Local Anesthetic Volume
Infraclavicular: 20-30 ml
Catheter Techniques
- The infraclavicular block facilitates excellent positioning of a continuous nerve block catheter with minimal risk of migration due to the “anchoring” of the catheter to the pectoralis minor and major muscles.
- Insert no more than 3-5 cm of the catheter into the brachial plexus sheath to prevent kinking or knotting of the catheter.
- Dermabond can be applied to the catheter insertion site to minimize “back leakage.”
- Continuous infraclavicular catheters infusions can initiate at 6-8 ml/hr and titrated accordingly.
Complications
- A phrenic nerve blockade can occur (< 10 % incidence) and is a relatively low risk complication for this block.
- Pneumothorax
- Hematoma
- Neural injury
- LAST (Local Anesthetic Toxicity)
PEARLS
- Careful attention should be made to location the depth and proximity of the pleura before performing the infraclavicular block by tilting the probe into the chest wall.
- This block can be painful, so generous localization of local anesthetic should be performed before needling begins.
- “Rocking” the probe can improve the angle of insonization with the needle for blocks that greater than 4 cm in depth. This maneuver brings the probe and needle into a more parallel alignment facilitating better needle tip visualization when performing deeper blocks in the infraclavicular region.
References
- Hebbard P, Royse C. Ultrasound guided posterior approach to the infraclavicular brachial plexus. Anaesthesia. 2007;62:539.
- Charbonneau J, Frechette Y, Sansoucy Y, Echave P. The ultrasound-guided retroclavicular block: A prospective feasibility study. Reg Anes Pain Med. 2015;40(5):605-609.
- Hadzic, Admir.Hadzic’s textbook of regional anesthesia and acute pain management. McGraw Hill Professional, 2017.
- Hebl, James R., and Robert L. Lennon, eds.Mayo Clinic Atlas of Regional Anesthesia and Ultrasound-Guided Nerve Blockade. Oxford University Press, 2010.